Lab 6: Muscular System I – Muscle Tissue and Hindlimb Muscles
Skeletal muscle cells and tissues, Muscles of the hindlimb
When you are prepared for the Test on Week 6-7 Learning Objectives in Week 8*, you will be able to:
- Identify components of a muscle cell and the neuromuscular junction.
- Identify connective tissues of muscles.
- Identify significant muscles on both human models and cats (listed in the lab activity).
- For the hamstrings, quadriceps and rotator cuff muscle groups: identify the muscles within them and the bony features that act as their attachment sites.
*Muscle dissections will span weeks 6-7. There will be no test in Week 7. In week 8, there will be a test covering all of the above learning objectives.
Muscle Tissue
When most people think of muscles, they think of the muscles that are visible just under the skin, particularly of the limbs. These are skeletal muscles, so-named because most of them move the skeleton. But as we learned in Week 3, there are two other types of muscle tissue in the body, with distinctly different jobs (Figure 6.1). Cardiac muscle, found in the heart, is concerned with pumping blood through the circulatory system. Smooth muscle is concerned with various involuntary movements, such as having one’s hair stand on end when cold or frightened, or moving food through the digestive system. In the next two weeks, we will focus on the structure and function of skeletal muscle tissue, and how it works with the skeletal system to move and stabilize the framework of the body. We will revisit cardiac and smooth muscle tissue later in the semester when looking at their roles in other organ systems.
Skeletal Muscle
The best-known feature of skeletal muscle is its ability to contract and cause movement. Skeletal muscles act not only to produce movement but also to stop movement, such as resisting gravity to maintain posture. Small, constant adjustments of the skeletal muscles are needed to hold a body upright or balanced in any position. Muscles also prevent excess movement of the bones and joints, maintaining skeletal stability and preventing skeletal structure damage or deformation. Joints can become misaligned or dislocated entirely by pulling on the associated bones; muscles work to keep joints stable. Skeletal muscles are located throughout the body at the openings of internal tracts to control the movement of various substances. These muscles allow functions, such as swallowing, urination, and defecation, to be under voluntary control. Skeletal muscles also protect internal organs (particularly abdominal and pelvic organs) by acting as an external barrier or shield to external trauma and by supporting the weight of the organs.
Skeletal muscles contribute to the maintenance of homeostasis in the body by generating heat. Muscle contraction requires energy, and when ATP is broken down, heat is produced. This heat is very noticeable during exercise, when sustained muscle movement causes body temperature to rise, and in cases of extreme cold, when shivering is caused by random skeletal muscle contractions to generate heat.
Each skeletal muscle is an organ that consists of various integrated tissues. These tissues include the skeletal muscle fibers, blood vessels, nerve fibers, and connective tissue. Skeletal muscles have three layers of connective tissue (called “mysia”, singular: “mysium”) that enclose it and provide structure to the muscle as a whole, and also compartmentalize the muscle fibers within the muscle (Figure 6.2). Each muscle is wrapped in connective tissue called the epimysium, which separates the muscle from other tissues and organs in the area, allowing the muscle to move independently.
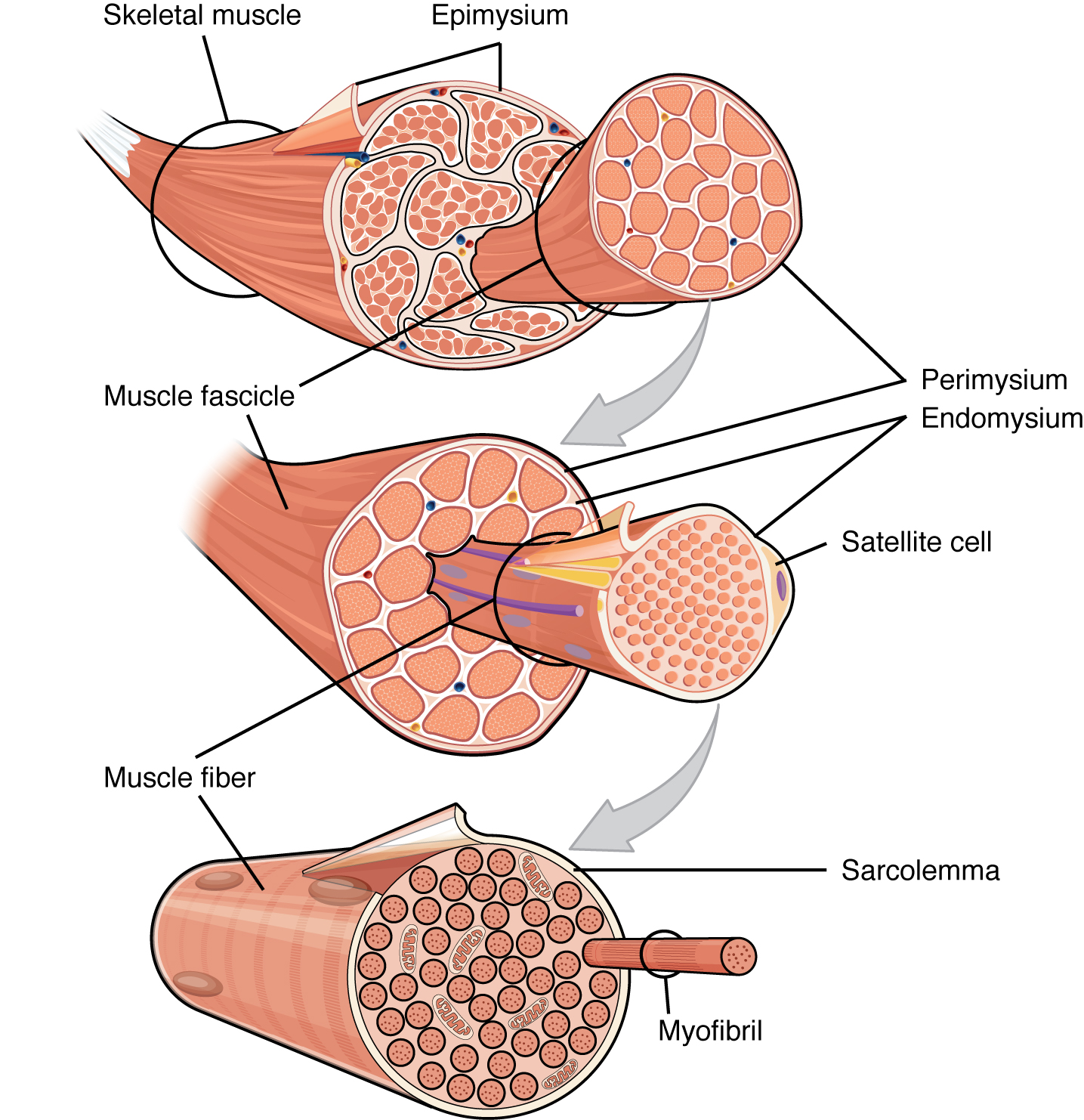
Inside each skeletal muscle, muscle fibers are organized into individual bundles, each called a fascicle, by a middle layer of connective tissue called the perimysium. This fascicular organization is common in muscles of the limbs; it allows the nervous system to trigger a specific movement of a muscle by activating a subset of muscle fibers within a bundle, or fascicle of the muscle. Inside each fascicle, each muscle fiber is encased in a thin connective tissue layer of collagen and reticular fibers called the endomysium. The endomysium contains the extracellular fluid and nutrients to support the muscle fiber. These nutrients are supplied via blood to the muscle tissue.
In skeletal muscles that work with tendons to pull on bones, the collagen in the three tissue layers (the mysia) intertwines with the collagen of a tendon. At the other end of the tendon, it fuses with the periosteum coating the bone. The tension created by contraction of the muscle fibers is then transferred though the mysia, to the tendon, and then to the periosteum to pull on the bone for movement of the skeleton. In other places, the mysia may fuse with a broad, tendon-like sheet called an aponeurosis, or to fascia, the connective tissue between skin and bones. The broad sheet of connective tissue in the lower back that the latissimus dorsi muscles (the “lats”) fuse into is an example of an aponeurosis.
Every skeletal muscle is also richly supplied by blood vessels for nourishment, oxygen delivery, and waste removal. In addition, every muscle fiber in a skeletal muscle is supplied by the axon branch of a somatic motor neuron, which signals the fiber to contract. Unlike cardiac and smooth muscle, the only way to functionally contract a skeletal muscle is through signaling from the nervous system.
Skeletal Muscle Fibers
Because skeletal muscle cells are long and cylindrical, they are commonly referred to as muscle fibers. Skeletal muscle fibers can be quite large for human cells, with diameters up to 100 μm and lengths up to 30 cm (11.8 in) in the Sartorius of the upper leg. During early development, embryonic myoblasts, each with its own nucleus, fuse with up to hundreds of other myoblasts to form the multinucleated skeletal muscle fibers. Multiple nuclei mean multiple copies of genes, permitting the production of the large amounts of proteins and enzymes needed for muscle contraction.
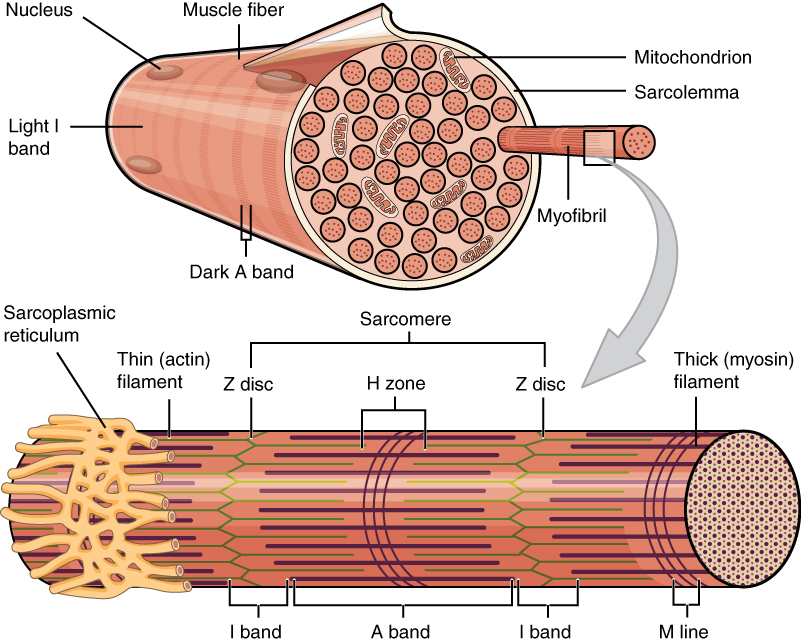
Some other terminology associated with muscle fibers is rooted in the Greek sarco, which means “flesh.” The plasma membrane of muscle fibers is called the sarcolemma, the cytoplasm is referred to as sarcoplasm, and the specialized smooth endoplasmic reticulum, which stores, releases, and retrieves calcium ions (Ca++) is called the sarcoplasmic reticulum (SR) (Figure 6.3). As will soon be described, the functional unit of a skeletal muscle fiber is the sarcomere, a highly organized arrangement of the contractile myofilaments actin (thin filament) and myosin (thick filament), along with other support proteins.
The Sarcomere
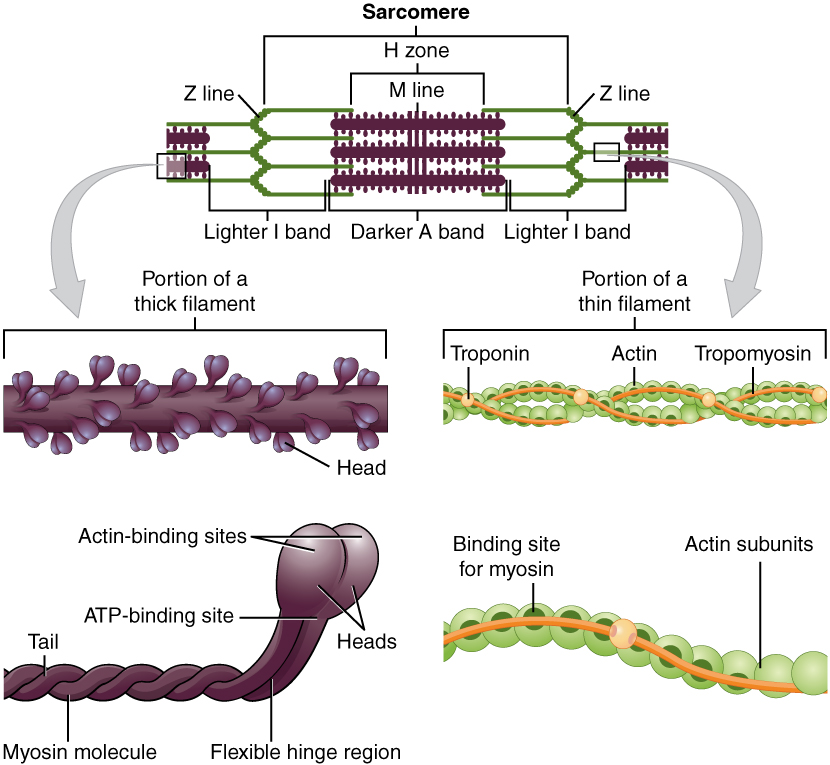
The striated appearance of skeletal muscle fibers is due to the arrangement of the myofilaments of actin and myosin in sequential order from one end of the muscle fiber to the other. Each packet of these microfilaments and their regulatory proteins, troponin and tropomyosin (along with other proteins) is called a sarcomere.
The sarcomere is the functional unit of the muscle fiber. The sarcomere itself is bundled within the myofibril that runs the entire length of the muscle fiber and attaches to the sarcolemma at its end. As myofibrils contract, the entire muscle cell contracts. Because myofibrils are only approximately 1.2 μm in diameter, hundreds to thousands (each with thousands of sarcomeres) can be found inside one muscle fiber. Each sarcomere is approximately 2 μm in length with a three-dimensional cylinder-like arrangement and is bordered by structures called Z-discs (also called Z-lines, because pictures are two-dimensional), to which the actin myofilaments are anchored (Figure 6.4). Because the actin form strands that are thinner than the myosin, it is called the thin filament of the sarcomere. Likewise, because the myosin strands and their multiple heads (projecting from the center of the sarcomere, toward but not all to way to, the Z-discs) have more mass and are thicker, they are called the thick filament of the sarcomere.
The Neuromuscular Junction and Muscle Contraction
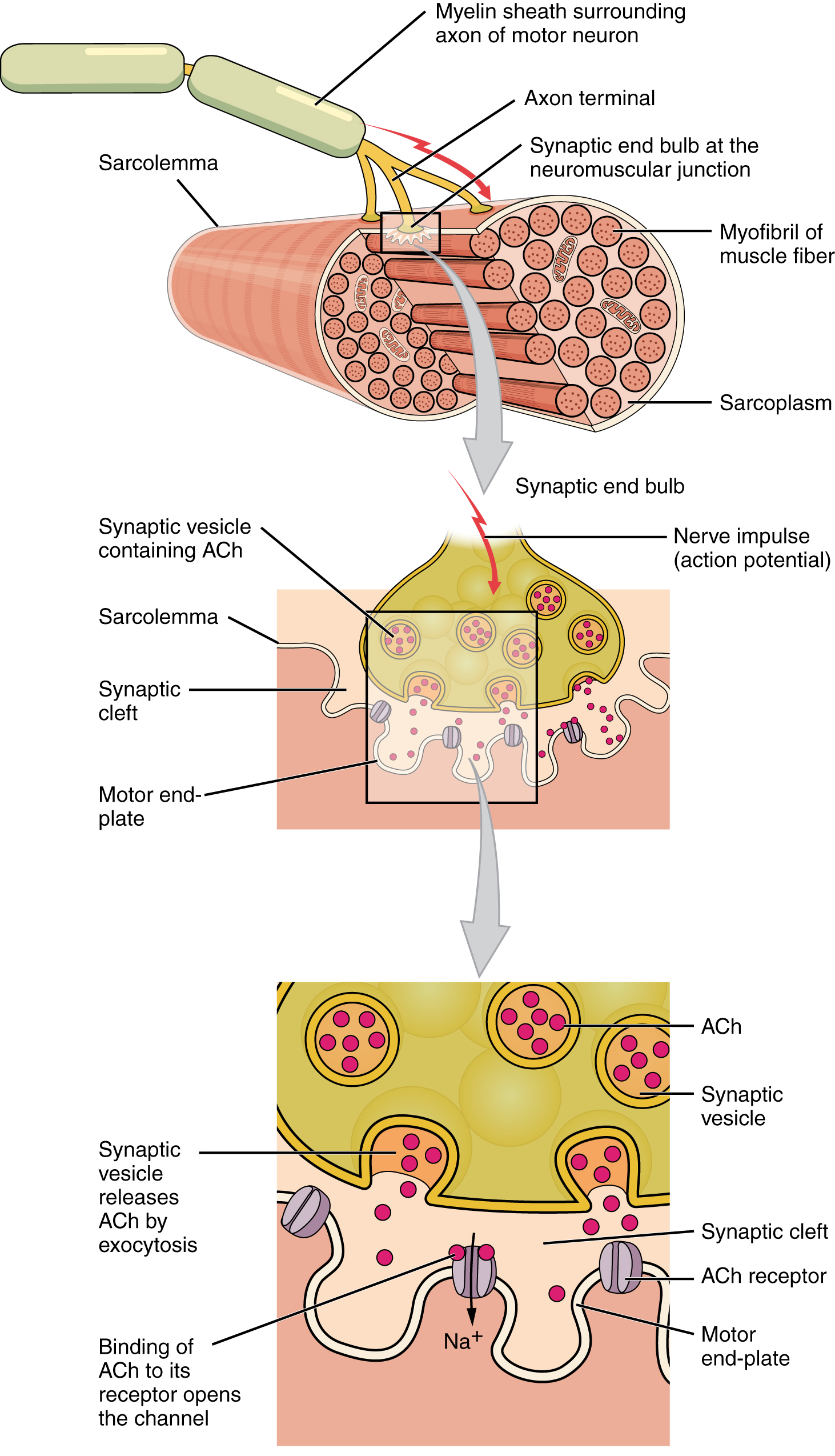
Another specialization of the skeletal muscle is the site where a motor neuron’s terminal meets the muscle fiber — called the neuromuscular junction (NMJ). This is where the muscle fiber first responds to signaling by the motor neuron. Every skeletal muscle fiber in every skeletal muscle is innervated by a motor neuron at the NMJ. Excitation signals from the neuron are the only way to functionally activate the fiber to contract.
All living cells have membrane potentials, or electrical gradients across their membranes. The inside of the membrane is usually around -60 to -90 mV, relative to the outside. This is referred to as a cell’s membrane potential. Neurons and muscle cells can use their membrane potentials to generate electrical signals. They do this by controlling the movement of charged particles, called ions, across their membranes to create electrical currents. This is achieved by opening and closing specialized proteins in the membrane called ion channels. Although the currents generated by ions moving through these channel proteins are very small, they form the basis of both neural signaling and muscle contraction.
Both neurons and skeletal muscle cells are electrically excitable, meaning that they are able to generate action potentials. An action potential is a special type of electrical signal that can travel along a cell membrane as a wave. This allows a signal to be transmitted quickly and faithfully over long distances.
For a skeletal muscle fiber to contract, its membrane must first be stimulated to fire an action potential. The muscle fiber action potential, which sweeps along the sarcolemma as a wave, causes contraction through the release of calcium ions (Ca++) from the SR. Once released, the Ca++ interacts with the shielding proteins, forcing them to move aside so that the actin-binding sites are available for attachment by myosin heads. The myosin then pulls the actin filaments toward the center, shortening the muscle fiber. In skeletal muscle, this sequence begins with signals from the somatic motor division of the nervous system. In other words, the “excitation” step in skeletal muscles is always triggered by signaling from the nervous system (Figure 6.5).
The motor neurons that tell the skeletal muscle fibers to contract originate in the spinal cord, with a smaller number located in the brainstem for activation of skeletal muscles of the face, head, and neck. These neurons have long processes, called axons, which are specialized to transmit action potentials long distances — in this case, all the way from the spinal cord to the muscle itself (which may be up to three feet away). The axons of multiple neurons bundle together to form nerves, like wires bundled together in a cable.
Signaling begins when a neuronal action potential travels along the axon of a motor neuron, and then along the individual branches to terminate at the NMJ. At the NMJ, the axon terminal releases a chemical messenger, or neurotransmitter, called acetylcholine (ACh). The ACh molecules diffuse across a minute space called the synaptic cleft and bind to ACh receptors located within the motor end-plate of the sarcolemma on the other side of the synapse. Once ACh binds, a channel in the ACh receptor opens and positively charged ions can pass through into the muscle fiber, causing it to depolarize, meaning that the membrane potential of the muscle fiber becomes less negative (closer to zero.)
As the membrane depolarizes, another set of ion channels called voltage-gated sodium channels are triggered to open. Sodium ions enter the muscle fiber, and an action potential rapidly spreads (or “fires”) along the entire membrane to initiate excitation-contraction coupling. Things happen very quickly in the world of excitable membranes (just think about how quickly you can snap your fingers as soon as you decide to do it). Immediately following depolarization of the membrane, it repolarizes, re- establishing the negative membrane potential. Meanwhile, the ACh in the synaptic cleft is degraded by the enzyme acetylcholinesterase (AChE) so that the ACh cannot rebind to a receptor and reopen its channel, which would cause unwanted extended muscle excitation and contraction.
Propagation of an action potential along the sarcolemma triggers the release of calcium ions (Ca2+) from its storage in the cell’s SR. For the action potential to reach the membrane of the SR, there are periodic invaginations in the sarcolemma, called T- tubules (“T” stands for “transverse”). You will recall that the diameter of a muscle fiber can be up to 100 μm, so these T-tubules ensure that the membrane can get close to the SR in the sarcoplasm. The arrangement of a T-tubule with the membranes of SR on either side is called a triad (Figure 6.6). The triad surrounds the cylindrical structure called a myofibril, which contains actin and myosin.
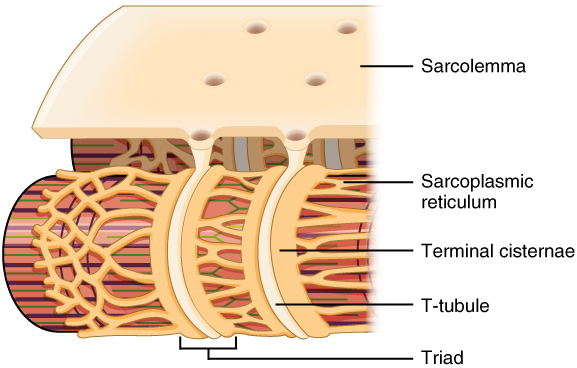
The T-tubules carry the action potential into the interior of the cell, which triggers the opening of calcium channels in the membrane of the adjacent SR, causing Ca++ to diffuse out of the SR and into the sarcoplasm. It is the arrival of Ca++ in the sarcoplasm that initiates contraction of the muscle fiber by its contractile units, or sarcomeres.
The Muscular System
Naming Skeletal Muscles
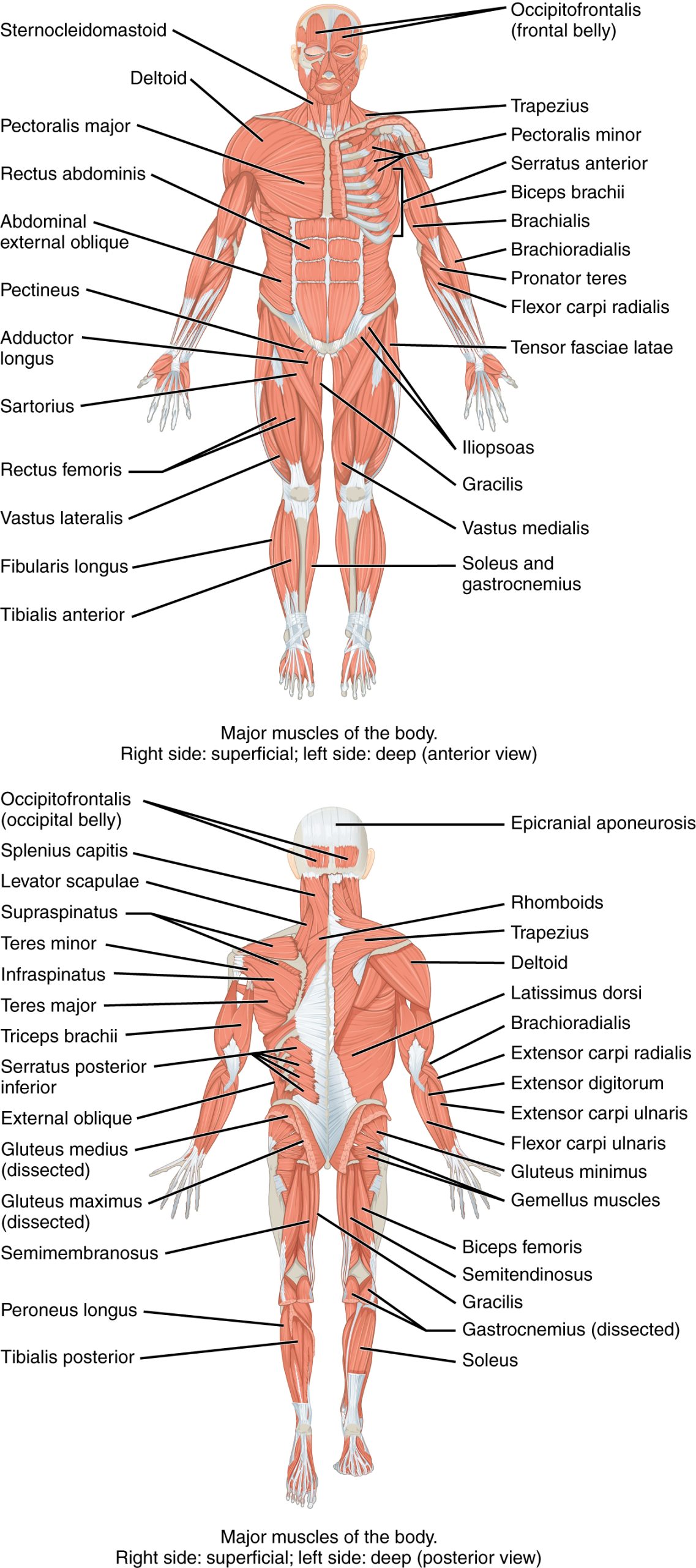
The Greeks and Romans conducted the first studies done on the human body in Western culture. The educated class of subsequent societies studied Latin and Greek, and therefore the early pioneers of anatomy continued to apply Latin and Greek terminology or roots when they named the skeletal muscles. The large number of muscles in the body and unfamiliar words can make learning the names of the muscles in the body seem daunting, but understanding the etymology can help. Etymology is the study of how the root of a particular word entered a language and how the use of the word evolved over time. Taking the time to learn the root of the words is crucial to understanding the vocabulary of anatomy and physiology. When you understand the names of muscles it will help you remember where the muscles are located and what they do (Figure 6.7 and Table 6.1). Pronunciation of words and terms will take a bit of time to master, but after you have some basic information; the correct names and pronunciations will become easier.
| Example | Word | Latin Roots |
Meaning | Translation |
| “abductor digiti minimi” | abductor | ab = away from; duct = to move | a muscle that moves away from | A muscle that moves the little finger or toe away |
| digiti | digitus = digit | a finger or toe | ||
| minimi | minimus = mini, tiny | little | ||
| “adductor digiti minimi” | adductor | ad = to, toward; duct = to move | a muscle that moves towards | A muscle that moves the little finger or toe toward |
| digiti | digitus = digit | a finger or toe | ||
| minimi | minimus = mini, tiny | little |
Anatomists name the skeletal muscles according to a number of criteria, each of which describes the muscle in some way. These include naming the muscle after its shape, its size compared to other muscles in the area, its location in the body or the location of its attachments to the skeleton, how many origins it has, or its action.
The skeletal muscle’s anatomical location or its relationship to a particular bone often determines its name. For example, the frontalis muscle is located on top of the frontal bone of the skull. Similarly, the shapes of some muscles are very distinctive and the names, such as orbicularis, reflect the shape. For the buttocks, the size of the muscles influences the names: gluteus maximus (largest), gluteus medius (medium), and the gluteus minimus (smallest). Names were given to indicate length—brevis (short), longus (long)—and to identify position relative to the midline: lateralis (to the outside away from the midline), and medialis (toward the midline). The direction of the muscle fibers and fascicles are used to describe muscles relative to the midline, such as the rectus (straight) abdominis, or the oblique (at an angle) muscles of the abdomen.
Some muscle names indicate the number of muscles in a group. One example of this is the quadriceps, a group of four muscles located on the anterior (front) thigh. Other muscle names can provide information as to how many origins a particular muscle has, such as the biceps brachii. The prefix bi indicates that the muscle has two origins and tri indicates three origins.
The location of a muscle’s attachment can also appear in its name. When the name of a muscle is based on the attachments, the origin is always named first. For instance, the sternocleidomastoid muscle of the neck has a dual origin on the sternum (sterno) and clavicle (cleido), and it inserts on the mastoid process of the temporal bone. The last feature by which to name a muscle is its action. When muscles are named for the movement they produce, one can find action words in their name. Some examples are flexor (decreases the angle at the joint), extensor (increases the angle at the joint), abductor (moves the bone away from the midline), or adductor (moves the bone toward the midline).
Skeletal Muscles by Region
The skeletal muscles are divided into axial (muscles of the trunk and head) and appendicular (muscles of the arms and legs) categories. This system reflects the bones of the skeleton system, which are also arranged in this manner. The axial and appendicular muscles are grouped based on location, function, or both. Some of the axial muscles may seem to blur the boundaries because they cross over to the appendicular skeleton.
In lab this week, we will look at the appendicular muscles in the hindlimb first because these are easiest to start with on our dissection. Next week we will continue exploring the skeletal muscles by region and look at the appendicular muscles in the forelimb and the axial muscles.
Appendicular Muscles of the Pelvic Girdle and Lower Limbs
The appendicular muscles of the lower body position and stabilize the pelvic girdle, which serves as a foundation for the lower limbs. Comparatively, there is much more movement at the pectoral girdle than at the pelvic girdle. There is very little movement of the pelvic girdle because of its connection with the sacrum at the base of the axial skeleton. The pelvic girdle is less range of motion because it was designed to stabilize and support the body.
Muscles of the Thigh
What would happen if the pelvic girdle, which attaches the lower limbs to the torso, were capable of the same range of motion as the shoulder girdle? For one thing, walking would expend more energy if the heads of the femurs were not secured in the acetabula of the pelvis. The body’s center of gravity is in the area of the pelvis. If the center of gravity were not to remain fixed, standing up would be difficult as well. Therefore, what the leg muscles lack in range of motion and versatility, they make up for in size and power, facilitating the body’s stabilization, posture, and movement.
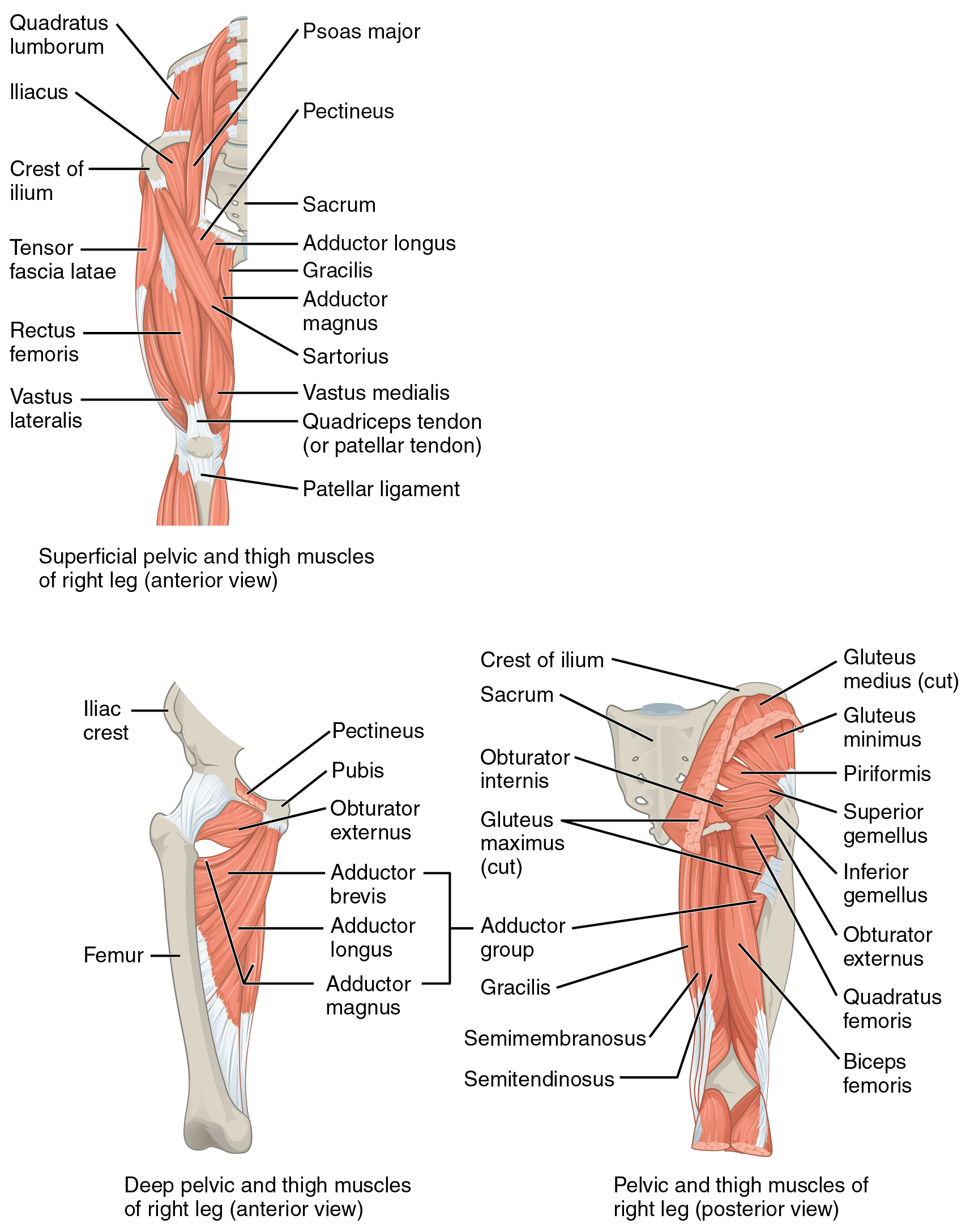
Gluteal Region Muscles That Move the Femur
Most muscles that insert on the femur (the thigh bone) and move it, originate on the pelvic girdle. The psoas major and iliacus make up the iliopsoas group. Some of the largest and most powerful muscles in the body are the gluteal muscles or gluteal group. The gluteus maximus is the largest; deep to the gluteus maximus is the gluteus medius, and deep to the gluteus medius is the gluteus minimus, the smallest of the trio (Figure 6.8 and Table 6.2).
| Group | Target | Movement | Target motion direction | Prime mover | Origin | Insertion |
| Iliopsoas group | femur | raises the knee at the hip, as if performing a knee attack; it also assists the lateral rotators in twisting the thigh (and lower leg) outward, and assists with bending over and maintaining posture | thigh: flexion and lateral rotation; torso: flexion |
psoas major | lumbar vertebrae (L1 through L5) and thoracic vertebra (T12) | lesser trochanter of femur |
| femur | raises the knee at the hip, as if performing a knee attack; it also assists the lateral rotators in twisting the thigh (and lower leg) outward, and assists with bending over and maintaining posture | thigh: flexion and lateral rotation; torso: flexion |
iliacus | iliac fossa, iliac crest, and lateral sacrum | lesser trochanter of femur | |
| Gluteal group | femur | lowers the knee and moves the thigh back, as when getting ready to kick a ball | extension | gluteous maximus | dorsal ilium, sacrum, and coccyx | gluteal tuberosity of femur; iliotibial tract |
| femur | opens the thigh, as when doing a split | abduction | gluteus medius | lateral surface of the ilium | greater trochanter of femur | |
| femur | brings the thighs back together | abduction | gluteus minimus | external surface of the ilium | greater trochanter of femur | |
| femur | assists with raising the knee at the hip and opening the thighs; it also maintains posture by stabilizing the iliotibial track, which connects to the knee | flexion; abduction | tensor fascia lata | anterior aspect of the iliac crest and the anterior superior iliac spine | iliotibial tract | |
| Lateral rotators | femur | twists the thigh (and lower leg) outward; it also maintains posture by stabilizing the hip joint | lateral rotation | piriformis | anterolateral surface of the sacrum | greater trochanter of femur |
| femur | twists the thigh (and lower leg) outward; it also maintains posture by stabilizing the hip joint | lateral rotation | obturator internus | inner surface of the obturator membrane, the greater sciatic notch, and the margins of the obturator foramen | greater trochanter in front of piriformis | |
| femur | twists thigh (and lower leg) outward; maintains posture by stabilizing hip joint | lateral rotation | obturator externus | outer surfaces of obturator membrane, pubic, and ischium; margins of obturator foramen | trochanteric fossa of posterior femur | |
| femur | twists the thigh (and lower leg) outward; it also maintains posture by stabilizing the hip joint | lateral rotation | superior gemellus | ischial spine | greater trochanter of femur | |
| femur | twists the thigh (and lower leg) outward; it also maintains posture by stabilizing the hip joint | lateral rotation | inferior gemellus | ischial tuberosity | greater trochanter of femur | |
| femur | twists the thigh (and lower leg) outward; it also maints posture by stabilizing the hip joint | lateral rotation | quatratus femoris | ischial tuberosity | trochanteric crest of femur | |
| Adductors | femur | brings the thighs back together; it also assists with raising the knee | adduction; flexion | adductor longus | pubis near the pubic symphysis | linea aspera |
| femur | brings the thighs back together; it also assists with raising the knee | adduction; flexion | adductor brevis | body of the pubis and in the inferior ramus of the pubis | linea aspera above adductor longus | |
| femur | brings the thighs back together; it also assists with raising the knee and moving the thigh back | adduction; flexion; extension | adductor magnus | ischial rami, the pubic rami, and the ischial tuberosity | linea aspera; adductor tubercle of femur | |
| femur | opens the thigh; with raising the knee and turning the thigh (and lower leg) inward | adduction; flexion; medial rotation | pectineus | pectineal line of the pubis | lesser trochanter to linea aspera of posterior aspect of femur |
The tensor fascia latae is a thick, squarish muscle in the superior aspect of the lateral thigh. It acts as a synergist of the gluteus medius and iliopsoas in flexing and abducting the thigh. It also helps stabilize the lateral aspect of the knee by pulling on the iliotibial tract (band), making it taut. Deep to the gluteus maximus, the piriformis, obturator internus, obturator externus, superior gemellus, inferior gemellus, and quadratus femoris laterally rotate the femur at the hip.
The adductor longus, adductor brevis, and adductor magnus can both medially and laterally rotate the thigh depending on the placement of the foot. The adductor longus flexes the thigh, whereas the adductor magnus extends it. The pectineus adducts and flexes the femur at the hip as well. The pectineus is located in the femoral triangle, which is formed at the junction between the hip and the leg and also includes the femoral nerve, the femoral artery, the femoral vein, and the deep inguinal lymph nodes.
Thigh Muscles That Move the Femur, Tibia, and Fibula
Deep fascia in the thigh separates it into medial, anterior, and posterior compartments (see Figure 6.8 and Table 6.3). The muscles in the medial compartment of the thigh are responsible for adducting the femur at the hip. Along with the adductor longus, adductor brevis, adductor magnus, and pectineus, the strap-like gracilis adducts the thigh in addition to flexing the leg at the knee.
| Group | Movement | Target | Target motion direction | Prime mover | Origin | Insertion |
| Medial compartment of thigh | moves the back of the lower legs up toward the buttocks, as when kneeling; it also assists in opening the thighs | femur; tibia/fibula | tibia/fibula: flexion; thigh: adduction |
gracilis | inferior ramus, the body of the pubis, and the ischial ramus | medial surface of tibia |
| Anterior compartment of the thigh: Quadriceps femoris group | moves the lower leg out in front of the body, as when kicking; it also assists in raising the knee | femur; tibia/fibula | tibia/fibula: extension; thigh: flexion |
rectus femoris | anterior inferior iliac spine and in the superior margin of the acetabulum | patella; tibial tuberosity |
| moves the lower leg out in front of the body, as when kicking | tibia/fibula | extension | vastus lateralis | greater trochanter, the intertrochanteric line, and the linea aspera | patella; tibial tuberosity | |
| moves the lower leg out in front of the body, as when kicking | tibia/fibula | extension | vastus medialis | linea aspera and the intertrochanteric line | patella; tibial tuberosity | |
| moves the lower leg out in front of the body, as when kicking | tibia/fibula | extension | vastus intermedius | proximal femur shaft | patella; tibial tuberosity | |
| moves the back of the lower legs up and back toward the buttocks, as when kneeling; it also assists in moving the thigh diagonally upward and outward as when mounting a bike | femur; tibia/fibula | tibia: flexion; thigh: flexion, abduction, lateral rotation |
sartorius | anterior superior iliac spine | medial aspect of proximal tibia | |
| Posterior compartment of the thigh: Hamstring group | moves the back of the lower leg up and back toward the buttocks, as when kneeling; it also moves the thigh down and back and twists the thigh (and lower leg) outward | femur; tibia/fibula | tibia/fibula: flexion; thigh: extension, lateral rotation |
biceps femoris | ischial tuberosity, linea aspera, and distal femur | head of fibula; lateral condyle of tibia |
| moves the back of the lower legs up toward the buttocks, as when kneeling; it also moves the thigh down and back and twists the thigh (and lower leg) inward | femur; tibia/fibula | tibia/fibula: flexion; thigh: extension, medial rotation |
semitendinosus | ischial tuberosity | upper tibial shaft | |
| moves the back of the lower legs up and back toward the buttocks, as when kneeling; it also moves the thigh down and back and twists the thigh (and lower leg) inward | femur; tibia/fibula | tibia/fibula: flexion; thigh: extension, medial rotation |
semimembranosus | ischial tuberosity | medial condyle of tibia; medial condyle of femur |
The muscles of the anterior compartment of the thigh flex the thigh and extend the leg. This compartment contains the quadriceps femoris group, which actually comprises four muscles that extend and stabilize the knee. The rectus femoris is on the anterior aspect of the thigh, the vastus lateralis is on the lateral aspect of the thigh, the vastus medialis is on the medial aspect of the thigh, and the vastus intermedius is between the vastus lateralis and vastus medialis and deep to the rectus femoris. The tendon common to all four is the quadriceps tendon (patellar tendon), which inserts into the patella and continues below it as the patellar ligament. The patellar ligament attaches to the tibial tuberosity. In addition to the quadriceps femoris, the sartorius is a band-like muscle that extends from the anterior superior iliac spine to the medial side of the proximal tibia. This versatile muscle flexes the leg at the knee and flexes, abducts, and laterally rotates the leg at the hip. This muscle allows us to sit cross-legged.
The posterior compartment of the thigh includes muscles that flex the leg and extend the thigh. The three long muscles on the back of the knee are the hamstring group, which flexes the knee. These are the biceps femoris, semitendinosus, and semimembranosus. The tendons of these muscles form the popliteal fossa, the diamond-shaped space at the back of the knee.
Muscles That Move the Feet and Toes
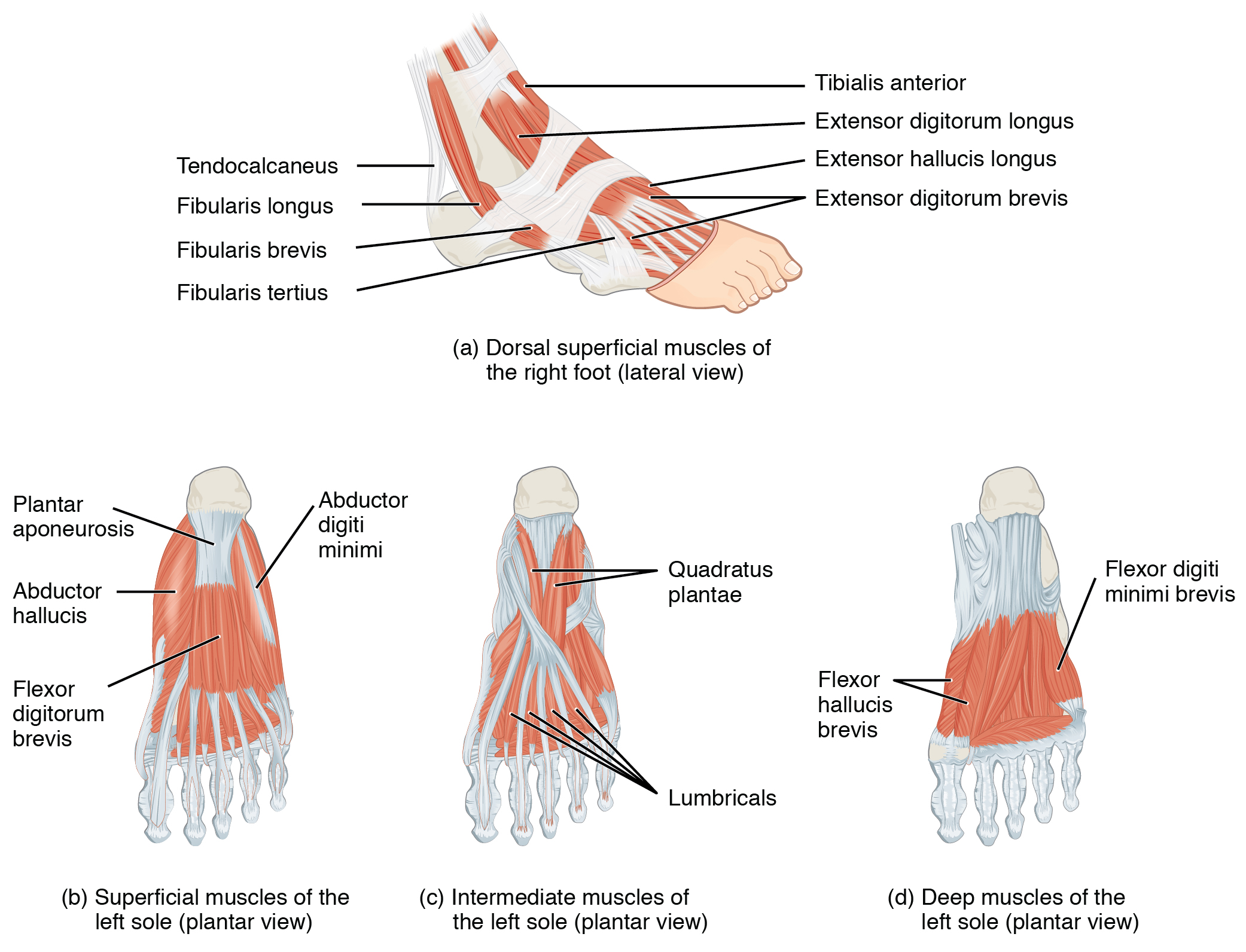
Similar to the thigh muscles, the muscles of the leg are divided by deep fascia into compartments, although the leg has three: anterior, lateral, and posterior (Figure 6.9 and Table 6.4).

| Group | Movement | Target | Target movement direction | Prime mover | Origin | Insertion |
| Anterior compartment of leg | Raises the sole of the foot off the ground, as when preparing to foot-tap; bends the inside of the foot upwards, as when catching your balance while falling laterally toward the opposite side as the balancing foot | foot | dorsiflexion; inversion | tibialis anterior | lateral condyle and upper tibial shaft; interosseous membrane | interior surface of medial cuneiform; first metatarsal bone |
| raises the sole of the foot off the ground, as when preparing to foot-tap; extends the big toe | foot; big toe | foot: dorsiflexion; big toe: extension |
extensor hallucis longus | anteromedial fibula shaft and interosseous membrane | distal phalanx of big toe | |
| raises the sole of the foot off the ground, as when preparing to foot-tap; extends the toes | foot; toes 2–5 | foot: dorsiflexion; toes: extension |
extensor digitorum longus | lateral condyle of the tibia, the proximal portion of the fibula, and the interosseous membrane | middle and distal phalanges of toes 2–5 | |
| Lateral compartment of leg | lowers the sole of the foot to the ground, as when foot-tapping or jumping; it also bends the inside of the foot downwards, as when catching your balance while falling laterally toward the same side as the balancing foot | foot | plantar flexion and eversion | fibularis longus | upper portion of the lateral fibula | first metatarsal; medial cuneiform |
| lowers the side of the foot to the ground, as when foot-tapping or jumping; it also bends the inside of the foot downward, as when catching your balance while falling laterally toward the same side as the balancing foot | foot | plantar flexion and eversion | fibularis (peroneus) brevis | distal fibula shaft | proximal end of fifth metatarsal | |
| Posterior compartment of leg: Superficial muscles | lowers the sole of the foot to the ground, as when foot-tapping or jumping; it also assists in moving the back of the lower legs up and back toward the buttocks | foot; tibia/fibula | foot: plantar flexion; tibia/fibula: flexion |
gastrocnemius | medial and lateral condyles of the femur | posterior calcaneus |
| lowers the sole of the foot the ground, as when foot-tapping or jumping; it also maintains posture while walking | foot | plantar flexion | soleus | superior tibia, fibula, and interosseous membrane | posterior calcaneus | |
| lowers the sole of the foot to the ground, as when foot-tapping or jumping; it also assists in moving the back of the lower legs up and back toward the buttocks | foot; tibia/fibula | foot: plantar flexion; tibia/fibula: flexion |
plantaris | posterior femur above the lateral condyle | calcaneus or calcaneus tendon | |
| lowers the sole of the foot to the ground, as when foot-tapping or jumping | foot | plantar flexion | tibialis posterior | superior tibia and fibula and in the interosseous membrane | several tarsals and metatarsals 2–4 | |
| Posterior compartment of leg: Deep muscles | moves the back of the lower legs up and back toward the buttocks; it also assists in rotation of the leg at the knee and thigh | tibia/fibula | tibia/fibula: flexion; thigh and lower leg: medial and lateral rotation |
popliteus | lateral condyle of the femur and the lateral meniscus | proximal tibia |
| lowers the sole of the foot to the ground, as when foot-tapping or jumping; it also bends the inside of the foot upward and flexes the toes | foot; toes 2–5 | foot: plantar flexion and inversion; toes: flexion |
flexor digitorum longus | posterior tibia | distal phalanges of toes 2–5 | |
| flexes the big toe | big toe; foot | big toe: flexion; foot: plantar flexion |
flexor hallicis longus | midshaft of fibula; interosseous membrane | distal phalanx of big toe |
The muscles in the anterior compartment of the leg: the tibialis anterior, a long and thick muscle on the lateral surface of the tibia, the extensor hallucis longus, deep under it, and the extensor digitorum longus, lateral to it, all contribute to raising the front of the foot when they contract. The fibularis tertius, a small muscle that originates on the anterior surface of the fibula, is associated with the extensor digitorum longus and sometimes fused to it, but is not present in all people. Thick bands of connective tissue called the superior extensor retinaculum (transverse ligament of the ankle) and the inferior extensor retinaculum, hold the tendons of these muscles in place during dorsiflexion.
The lateral compartment of the leg includes two muscles: the fibularis longus (peroneus longus) and the fibularis brevis (peroneus brevis). The superficial muscles in the posterior compartment of the leg all insert onto the calcaneal tendon (Achilles tendon), a strong tendon that inserts into the calcaneal bone of the ankle. The muscles in this compartment are large and strong and keep humans upright. The most superficial and visible muscle of the calf is the gastrocnemius. Deep to the gastrocnemius is the wide, flat soleus. The plantaris runs obliquely between the two; some people may have two of these muscles, whereas no plantaris is observed in about seven percent of other cadaver dissections. The plantaris tendon is a desirable substitute for the fascia lata in hernia repair, tendon transplants, and repair of ligaments. There are four deep muscles in the posterior compartment of the leg as well: thepopliteus, flexor digitorum longus, flexor hallucis longus, and tibialis posterior.
The foot also has intrinsic muscles, which originate and insert within it (similar to the intrinsic muscles of the hand). These muscles primarily provide support for the foot and its arch, and contribute to movements of the toes (Figure 6.10 and Table 6.5). The principal support for the longitudinal arch of the foot is a deep fascia called plantar aponeurosis, which runs from the calcaneus bone to the toes (inflammation of this tissue is the cause of “plantar fasciitis,” which can affect runners. The intrinsic muscles of the foot consist of two groups. The dorsal group includes only one muscle, the extensor digitorum brevis. The second group is the plantar group, which consists of four layers, starting with the most superficial.
| Group | Movement | Target | Target motion direction | Primve mover | Origin | Insertion |
| Dorsal group | extends toes 2 through 5 | toes 2–5 | extension | extensor digitorum brevis | calcaneus; extensor retinaculum | base of proximal phalanx of big toe; extensor expansions on toes 2–5 |
| Plantar group (layer 1) | abducts and flexes the big toe | big toe | adduction; flexion | abductor hallucis | calcaneal tuberosity; flexor retinaculum | proximal phalanx of big toe |
| flexes toes 2 through 4 | middle toes | flexion | flexor digitorum brevis | calcaneal tuberosity | middle phalanx of toes 2–4 | |
| abducts and flexes the small toe | toe 5 | abduction; flexion | abductor digiti minimi | calcaneal tuberosity | proximal phalanx of little toe | |
| Plantar group (layer 2) | assists in flexing toes 2-5 | toes 2–5 | flexion | quadratus plantae | medial and lateral sides of calcaneus | tendon of flexor digitorum longus |
| extends toes 2-5 at the interphalangeal joints; flexes the small toes at the metatarsophalnageal joints | toes 2–5 | extension; flexion | lumbricals | tendons of flexor digitorum longus | medial side of proximal phalanx of toes 2-5 | |
| Plantar group (layer 3) | flexes the big toe | big toe | flexion | flexor hallucis brevis | lateral cuneiform; cuboid bones | base of proximal phalanx of big toe |
| adducts and flexes the big toe | big toe | adduction; flexion | adductor hallucis | bases of metatarsals 2 through 4; fibularis longus tendon sheath; ligament across the metatarsophalangeal joints | base of proximal phalanx of big toe | |
| flexes the small toe | little toe | flexion | flexor digiti minimi brevis | base of metatarsal 5; tendon sheath of the fibularis longus | base of proximal phalanx of little toe | |
| Plantar group (layer 4) | abducts and flexes the middle toes at the metatarsophalangeal joints; it also extends the middle toes at the interphalangeal joints | middle toes | abduction; flexion; extension | dorsal interossei | sides of the metatarsals | both sides of toe 2; for each tother to, extensor expansion over first phalanx on side opposite toe 2 |
| abducts toes 3 through 5; it also flexes the proximal phalanges and extends the distal phalanges | small toes | abduction; flexion; extension | plantar interossei | side of each metatarsal that faces metatarsal 2 (absent from metatarsal 2) | extensor expansion on first phalanx of each toe (except toe 2) on side facing toe 2 |

