Lab 13: Endocrine system & Digestive system
When you are prepared for the Test on Week 13 Learning Objectives in Week 14, you will be able to:
- Identify endocrine glands and describe their basic functions.
- Identify major structures and organs of the digestive system and their functions.
- Identify structures of teeth and classify teeth as incisors, canines, premolars, and molars.
- Identify absorptive structures of the small intestine.
- Identify mesentery structures and peritoneal attachments of abdominal organs.
- Describe the pathway that food takes through the primary organs of the digestive system.
- Describe the pathways of bile and pancreatic enzymes to the small intestine.
The Endocrine System
Communication is a process in which a sender transmits signals to one or more receivers to control and coordinate actions. In the human body, two major organ systems participate in relatively “long distance” communication: the nervous system and the endocrine system. Together, these two systems are primarily responsible for maintaining homeostasis in the body.
The nervous system uses two types of intercellular communication, electrical signaling (action potentials) and chemical signaling (neurotransmitters) that results in rapid signaling through the body. The target cell of the nervous system responds within milliseconds of receiving the chemical “message”; this response then ceases very quickly once the neural signaling ends. In this way, neural communication enables body functions that involve quick, brief actions, such as movement, sensation, and cognition. In contrast, the endocrine system uses just one method of communication: chemical signaling. These signals are sent by the endocrine organs, which secrete chemicals—the hormone—into the extracellular fluid. Hormones are transported primarily via the bloodstream throughout the body, where they bind to receptors on target cells, inducing a characteristic response. As a result, endocrine signaling requires more time than neural signaling to prompt a response in target cells, though the precise amount of time varies with different hormones. For example, the hormones released when you are confronted with a dangerous or frightening situation, called the fight-or-flight response, occur by the release of adrenal hormones—epinephrine and norepinephrine—within seconds. In contrast, it may take up to 48 hours for target cells to respond to certain reproductive hormones.
Although a given hormone may travel throughout the body in the bloodstream, it will affect the activity only of its target cells; that is, cells with receptors for that particular hormone. Once the hormone binds to the receptor, a chain of events is initiated that leads to the target cell’s response. Hormones play a critical role in the regulation of physiological processes because of the target cell responses they regulate. These responses contribute to human reproduction, growth and development of body tissues, metabolism, fluid, and electrolyte balance, sleep, and many other body functions. The major hormones of the human body and their effects are identified in Table 13.1.
| Endocrine gland | Associated hormones | Effect |
|---|---|---|
| Pituitary (anterior) | Growth hormone (GH) | Promotes growth of body tissues |
| Pituitary (anterior) | Prolactin (PRL) | Promotes milk production |
| Pituitary (anterior) | Thyroid-stimulating hormone (TSH) | Stimulates thyroid hormone release |
| Pituitary (anterior) | Adrenocorticotropic hormone (ACTH) | Stimulates hormone release by adrenal cortex |
| Pituitary (anterior) | Follicle-stimulating hormone (FSH) | Stimulates gamete production |
| Pituitary (anterior) | Luteinizing hormone (LH) | Stimulates androgen production by gonads |
| Pituitary (posterior) | Antidiuretic hormone (ADH) | Stimulates water reabsorption by kidneys |
| Pituitary (posterior) | Oxytocin | Stimulates uterine contractions during childbirth |
| Thyroid | Thyroxine (T4), triiodothyronine (T3) | Stimulate basal metabolic rate |
| Thyroid | Calcitonin | Reduces blood Ca2+ levels |
| Parathyroid | Parathyroid hormone (PTH) | Increases blood Ca2+ levels |
| Adrenal (cortex) | Aldosterone | Increases blood Na+ levels |
| Adrenal (cortex) | Cortisol, corticosterone, cortisone | Increase blood glucose levels |
| Adrenal (medulla) | Epinephrine, norepinephrine | Stimulate fight-or-flight response |
| Pineal | Melatonin | Regulates sleep cycles |
| Pancreas | Insulin | Reduces blood glucose levels |
| Pancreas | Glucagon | Increases blood glucose levels |
| Testes | Testosterone | Stimulates development of male secondary sex characteristics and sperm production |
| Ovaries | Estrogens and progesterone | Stimulate development of female secondary sex characteristics and prepare the body for childbirth |
Structures of the Endocrine System
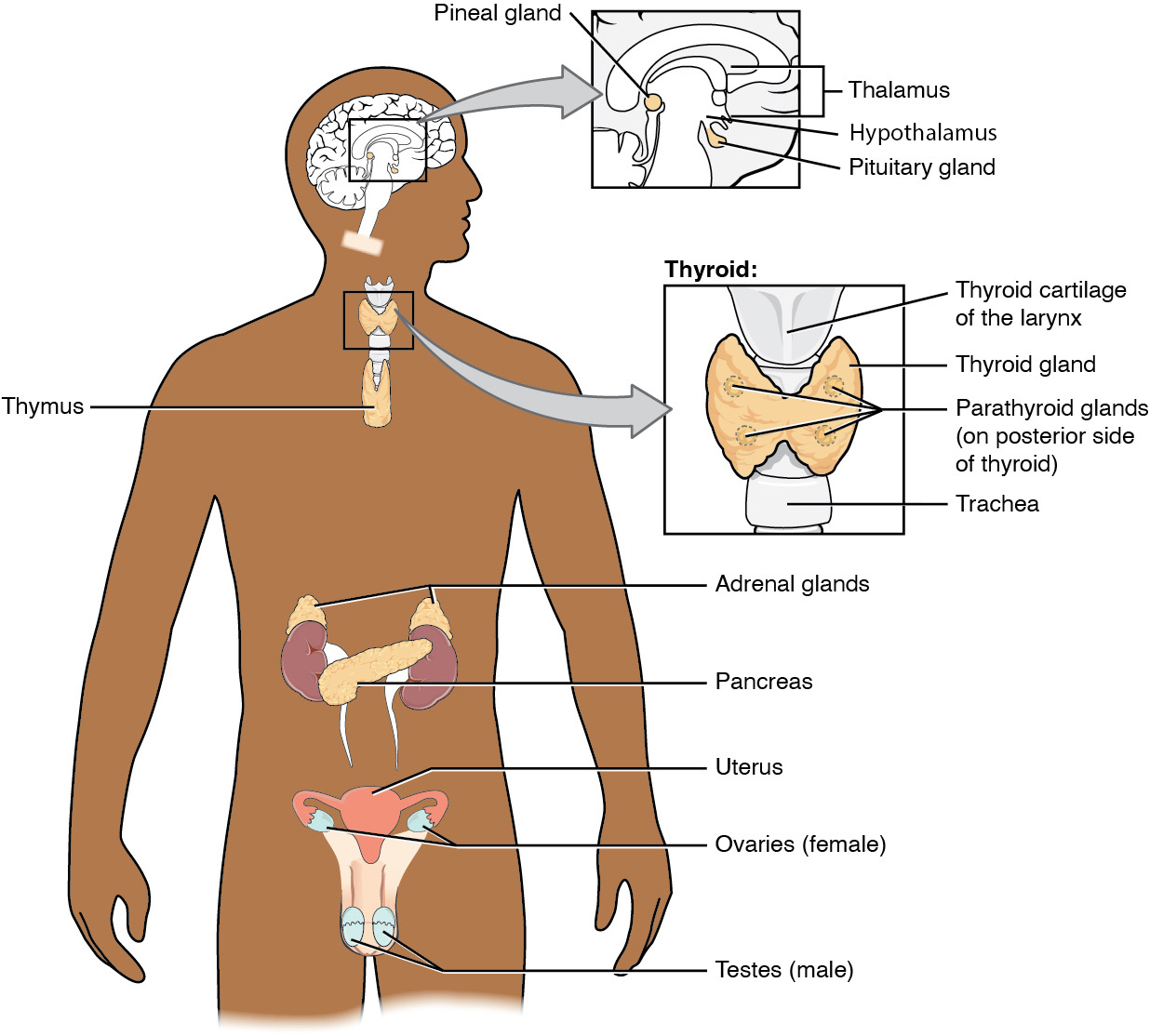
The endocrine system consists of cells, tissues, and organs that secrete hormones as a primary or secondary function (Figure 13.1). The endocrine gland is the major player in this system. The primary function of these ductless glands is to secrete their hormones directly into the surrounding fluid. The interstitial fluid and the blood vessels then transport the hormones throughout the body. The endocrine system includes the pituitary, thyroid, parathyroid, adrenal, and pineal glands. Some of these glands have both endocrine and non-endocrine functions. For example, the pancreas contains cells that function in digestion as well as cells that secrete the hormones insulin and glucagon, which regulate blood glucose levels. The hypothalamus, thymus, heart, kidneys, stomach, small intestine, liver, skin, female ovaries, and male testes are other organs that contain cells with endocrine function. Moreover, adipose tissue has long been known to produce hormones, and recent research has revealed that even bone tissue has endocrine functions.
The ductless endocrine glands are not to be confused with the body’s exocrine system, whose glands release their secretions through ducts. Examples of exocrine glands include the sebaceous and sweat glands of the skin. As just noted, the pancreas also has an exocrine function: most of its cells secrete pancreatic juice through the pancreatic and accessory ducts to the lumen of the small intestine.
The pituitary gland and hypothalamus
The hypothalamus–pituitary complex can be thought of as the “command center” of the endocrine system. This complex secretes several hormones that directly produce responses in target tissues, as well as hormones that regulate the synthesis and secretion of hormones of other glands. In addition, the hypothalamus–pituitary complex coordinates the messages of the endocrine and nervous systems. In many cases, a stimulus received by the nervous system must pass through the hypothalamus–pituitary complex to be translated into hormones that can initiate a response.
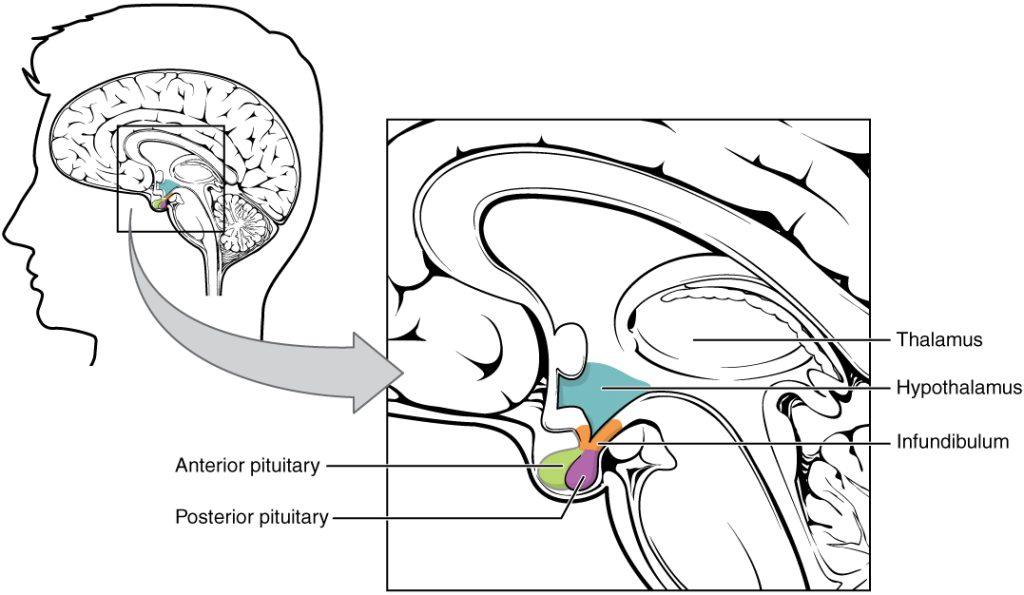
The hypothalamus is a structure of the diencephalon of the brain located anterior and inferior to the thalamus (Figure 13.2). It has both neural and endocrine functions, producing and secreting many hormones. In addition, the hypothalamus is anatomically and functionally related to the pituitary gland (or hypophysis), a bean-sized organ suspended from it by a stem called the infundibulum (or pituitary stalk). The pituitary gland is cradled within the sella turcica of the sphenoid bone of the skull. It consists of two lobes that arise from distinct parts of embryonic tissue: the posterior pituitary (neurohypophysis) is neural tissue, whereas the anterior pituitary (also known as the adenohypophysis) is glandular tissue that develops from the primitive digestive tract.
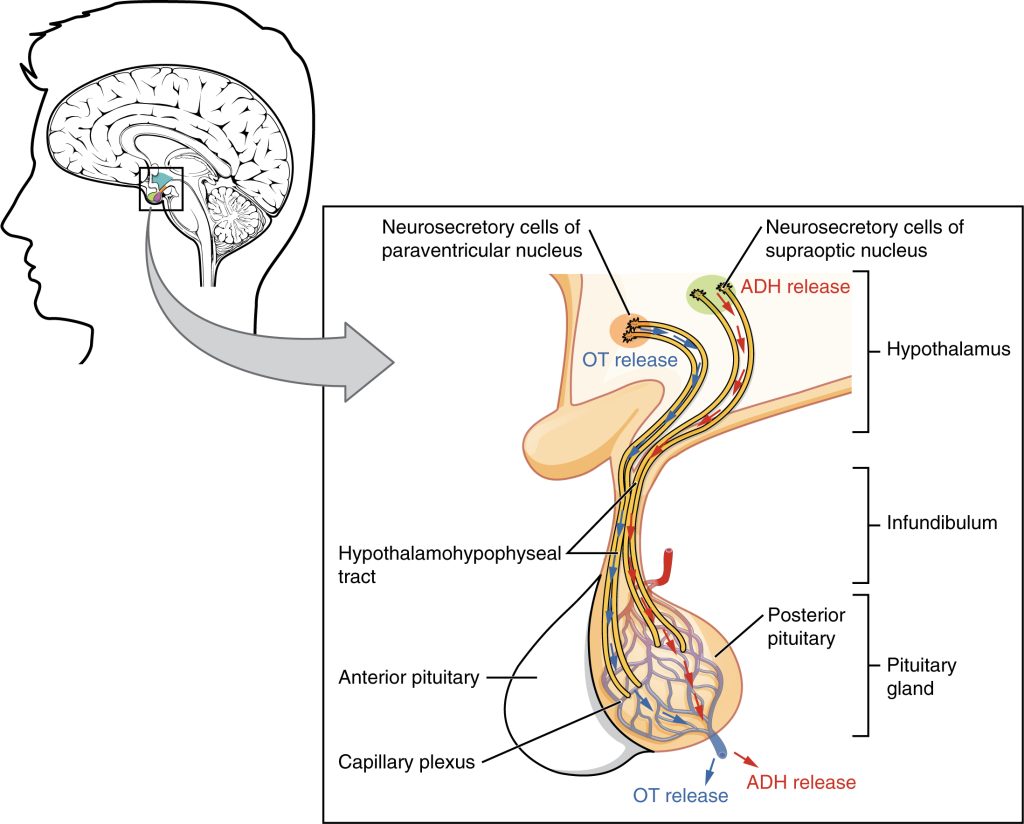
The posterior pituitary is actually an extension of the neurons in the hypothalamus. The cell bodies of these neurons rest in the hypothalamus, but their axons descend as the hypothalamic–hypophyseal tract within the infundibulum, and end in axon terminals that comprise the posterior pituitary. The posterior pituitary gland does not produce hormones, but rather stores and secretes hormones produced by the hypothalamus, including oxytocin and ADH (Figure 13.3).
In contrast to the posterior pituitary, the anterior pituitary does manufacture hormones. However, the secretion of hormones from the anterior pituitary is regulated by two classes of hormones secreted by the hypothalamus, the releasing hormones that stimulate the secretion, and the inhibiting hormones that inhibit secretion.
Hypothalamic releasing and inhibiting hormones are secreted by neurons, but enter the anterior pituitary through blood vessels. Within the infundibulum is a bridge of capillaries that connects the hypothalamus to the anterior pituitary. This network, called the hypophyseal portal system, allows hypothalamic hormones to be transported to the anterior pituitary without first entering the systemic circulation. Hormones produced by the anterior pituitary (in response to releasing hormones) enter a secondary capillary plexus, and from there drain into the circulation.
The anterior pituitary produces seven hormones. These are the growth hormone (GH), thyroid-stimulating hormone (TSH), adrenocorticotropic hormone (ACTH), follicle-stimulating hormone (FSH), luteinizing hormone (LH), beta endorphin, and prolactin. Of the hormones of the anterior pituitary, TSH, ACTH, FSH, and LH are collectively referred to as tropic hormones (trope- = “turning”) because they turn on or off the function of other endocrine glands. The hormones secreted by the pituitary gland are summarized in Table 13.1.
The thyroid and parathyroid glands
A butterfly-shaped organ, the thyroid gland is located anterior to the trachea, just inferior to the larynx (Figure 13.4). The medial region, called the isthmus, is flanked by wing-shaped left and right lobes. Each of the thyroid lobes are embedded with parathyroid glands, primarily on their posterior surfaces. The tissue of the thyroid gland is composed mostly of thyroid follicles, where thyroid hormones are produced. There are two types of thyroid hormone, triiodothyronine (T3) and thyroxine (T4), which both influence the body’s basal metabolic rate. The thyroid gland also secretes a hormone called calcitonin, which helps regulate calcium concentrations in the blood along with parathyroid hormone.
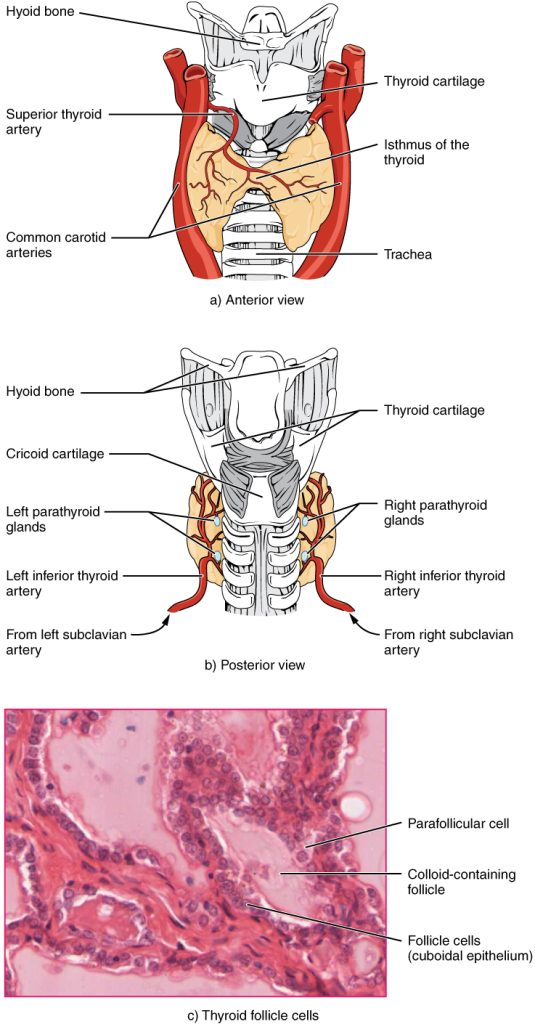
The parathyroid glands are tiny, round structures usually found embedded in the posterior surface of the thyroid gland (Figure 13.4). A thick connective tissue capsule separates the glands from the thyroid tissue. Most people have four parathyroid glands, but occasionally there are more in tissues of the neck or chest. The parathyroid glands produce and secrete the parathyroid hormone (PTH), the major hormone involved in the regulation of blood calcium levels.
The adrenal glands
The adrenal glands are wedges of glandular and neuroendocrine tissue adhering to the top of the kidneys by a fibrous capsule (Figure 13.5). The adrenal gland consists of an outer cortex of glandular tissue and an inner medulla of nervous tissue. The adrenal glands have a rich blood supply and experience one of the highest rates of blood flow in the body. They are served by several arteries branching off the aorta, including the suprarenal and renal arteries. Adrenal hormones are released into the circulation via the left and right suprarenal veins.
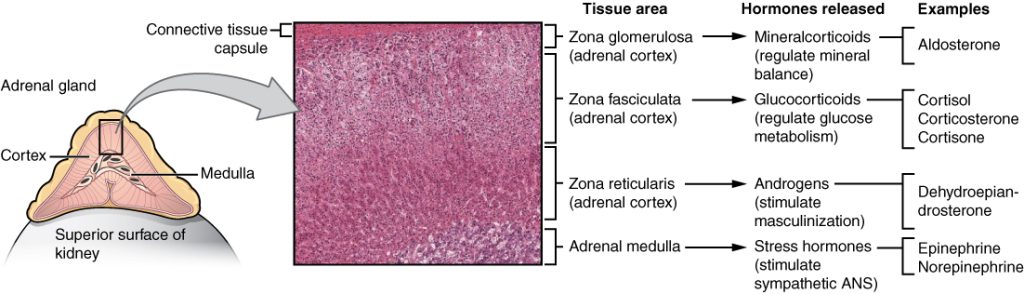
The adrenal cortex is divided into three zones: the zona glomerulosa, the zona fasciculata, and the zona reticularis. Each region secretes its own set of hormones, involved in functions such as the regulation of the long-term stress response, blood pressure and blood volume, nutrient uptake and storage, fluid and electrolyte balance, and inflammation.
The adrenal medulla is neuroendocrine tissue composed of postganglionic sympathetic nervous system neurons. It is really an extension of the autonomic nervous system, which regulates homeostasis in the body. The medulla is stimulated to secrete the hormones epinephrine and norepinephrine.
The endocrine functions of the pancreas
The pancreas is a long, slender organ, most of which is located posterior to the bottom half of the stomach (Figure 13.6). Although it is primarily an exocrine gland, secreting a variety of digestive enzymes, the pancreas has an endocrine function. Its pancreatic islets—clusters of cells formerly known as the islets of Langerhans—secrete the hormones glucagon, insulin, somatostatin, and pancreatic polypeptide (PP). Most of these hormones are involved in the regulation of blood glucose levels.
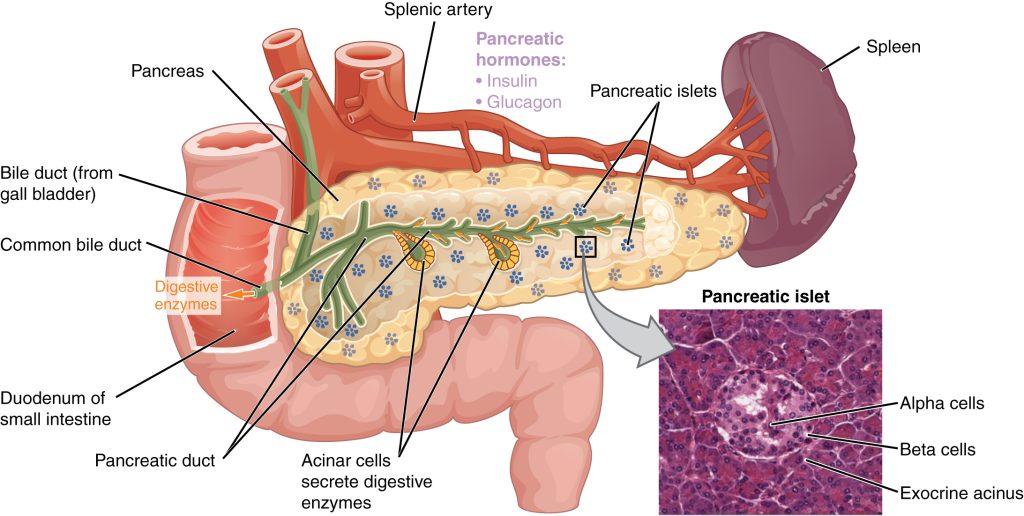
Glucose is required for cellular respiration and is the preferred fuel for all body cells. The body derives glucose from the breakdown of the carbohydrate-containing foods and drinks we consume. Glucose not immediately taken up by cells for fuel can be stored by the liver and muscles as glycogen, or converted to triglycerides and stored in the adipose tissue. Hormones regulate both the storage and the utilization of glucose as required. Receptors located in the pancreas sense blood glucose levels, and subsequently the pancreatic cells secrete glucagon or insulin to maintain normal levels.
Other organs involved with the endocrine system
The pineal gland is located in the diencephalon of the brain, along the inferoposterior edge. It is a tiny endocrine gland that produces and secretes the hormone melatonin, which is involved in the sleep-wake cycle of the body.
The gonads, the male testes and female ovaries, produce the sex cells (sperm and ova) and secrete the gonadal hormones. The primary hormone produced by the male testes is testosterone, a steroid hormone important in the development of the male reproductive system, the maturation of sperm cells, and the development of male secondary sex characteristics. The primary hormones produced by the ovaries are estrogens, which play an important role in the development of the female reproductive system, regulation of the menstrual cycle, the development of female secondary sex characteristics, and the maintenance of pregnancy. Another significant ovarian hormone is progesterone, which contributes to regulation of the menstrual cycle and is important in preparing the body for pregnancy as well as maintaining pregnancy.
During the initial stages of pregnancy, an organ called the placenta develops within the uterus. The placenta supplies oxygen and nutrients to the fetus, excretes waste products, and produces and secretes estrogens and progesterone. The placenta also produces human chorionic gonadotropin (hCG), which helps maintain pregnancy.
The heart, gastrointestinal tract, kidneys, skeleton, adipose tissue, skin, and thymus all have secondary endocrine functions, meaning they produce hormones apart from their primary function. The major hormones of these organs are summarized in Table 13.2.
| Organ | Major hormones | Effects |
|---|---|---|
| Heart | Atrial natriuretic peptide (ANP) | Reduces blood volume, blood pressure, and Na+ concentration |
| Gastrointestinal tract | Gastrin, secretin, and cholecystokinin | Aid digestion of food and buffering of stomach acids |
| Gastrointestinal tract | Glucose-dependent insulinotropic peptide (GIP) and glucagon-like peptide 1 (GLP-1) | Stimulate beta cells of the pancreas to release insulin |
| Kidneys | Renin | Stimulates release of aldosterone |
| Kidneys | Calcitriol | Aids in the absorption of Ca2+ |
| Kidneys | Erythropoietin | Triggers the formation of red blood cells in the bone marrow |
| Skeleton | FGF23 | Inhibits production of calcitriol and increases phosphate excretion |
| Skeleton | Osteocalcin | Increases insulin production |
| Adipose tissue | Leptin | Promotes satiety signals in the brain |
| Adipose tissue | Adiponectin | Reduces insulin resistance |
| Skin | Cholecalciferol | Modified to form vitamin D |
| Thymus (and other organs) | Thymosins | Among other things, aids in the development of T lymphocytes of the immune system |
| Liver | Insulin-like growth factor-1 | Stimulates bodily growth |
| Liver | Angiotensinogen | Raises blood pressure |
| Liver | Thrombopoietin | Causes increase in platelets |
| Liver | Hepcidin | Blocks release of iron into body fluids |
The Digestive System
The digestive system is continually at work, yet people seldom appreciate the complex tasks it performs in a choreographed biologic symphony. Consider what happens when you eat an apple. Of course, you enjoy the apple’s taste as you chew it, but in the hours that follow, unless something goes amiss and you get a stomachache, you don’t notice that your digestive system is working. You may be taking a walk or studying or sleeping, having forgotten all about the apple, but your stomach and intestines are busy digesting it and absorbing its vitamins and other nutrients. By the time any waste material is excreted, the body has appropriated all it can use from the apple. In short, whether you pay attention or not, the organs of the digestive system perform their specific functions, allowing you to use the food you eat to keep you going. This chapter examines the structure and functions of these organs, and explores the mechanics and chemistry of the digestive processes.
The function of the digestive system is to break down the foods you eat, release their nutrients, and absorb those nutrients into the body. Although the small intestine is the workhorse of the system, where the majority of digestion occurs, and where most of the released nutrients are absorbed into the blood or lymph, each of the digestive system organs makes a vital contribution to this process (Figure 13.7).
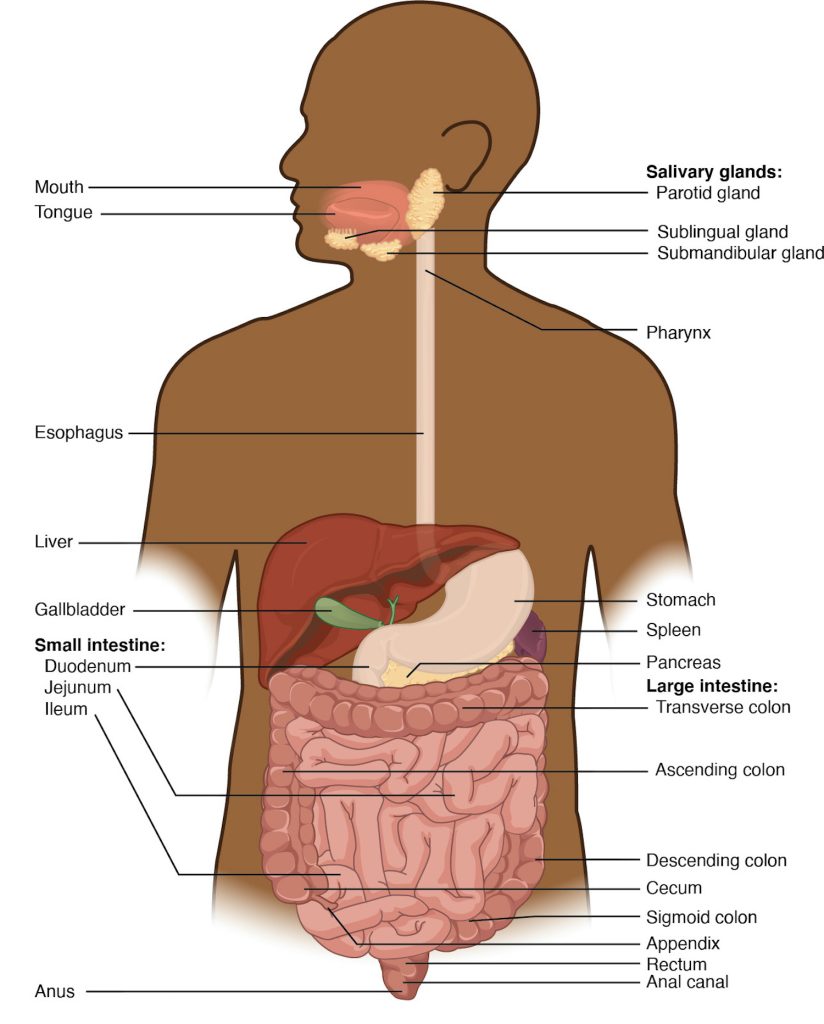
The easiest way to understand the digestive system is to divide its organs into two main categories. The first group is the organs that make up the alimentary canal. Accessory digestive organs comprise the second group and are critical for orchestrating the breakdown of food and the assimilation of its nutrients into the body. Accessory digestive organs, despite their name, are critical to the function of the digestive system.
Alimentary Canal Organs
Also called the gastrointestinal (GI) tract or gut, the alimentary canal (aliment- = “to nourish”) is a one-way tube about 7.62 meters (25 feet) in length during life and closer to 10.67 meters (35 feet) in length when measured after death, once smooth muscle tone is lost. The main function of the organs of the alimentary canal is to nourish the body. This tube begins at the mouth and terminates at the anus. Between those two points, the canal is modified as the pharynx, esophagus, stomach, and small and large intestines to fit the functional needs of the body. Both the mouth and anus are open to the external environment; thus, food and wastes within the alimentary canal are technically considered to be outside the body. Only through the process of absorption do the nutrients in food enter into and nourish the body’s “inner space.”
Accessory Structures
Each accessory digestive organ aids in the breakdown of food. Within the mouth, the teeth and tongue begin mechanical digestion, whereas the salivary glands begin chemical digestion. Once food products enter the small intestine, the gallbladder, liver, and pancreas release secretions—such as bile and enzymes—essential for digestion to continue. Together, these are called accessory organs because they sprout from the lining cells of the developing gut (mucosa) and augment its function; indeed, you could not live without their vital contributions, and many significant diseases result from their malfunction. Even after development is complete, they maintain a connection to the gut by way of ducts.
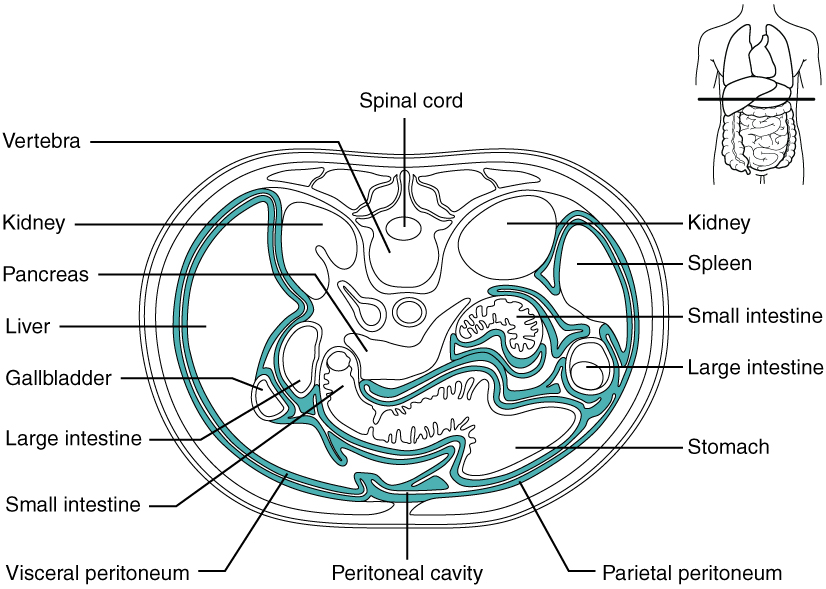
The Peritoneum
The digestive organs within the abdominal cavity are held in place by the peritoneum, a broad serous membranous sac made up of squamous epithelial tissue surrounded by connective tissue. It is composed of two different regions: the parietal peritoneum, which lines the abdominal wall, and the visceral peritoneum, which envelopes the abdominal organs (Figure 13.8). The peritoneal cavity is the space bounded by the visceral and parietal peritoneal surfaces. A few milliliters of watery fluid act as a lubricant to minimize friction between the serosal surfaces of the peritoneum.
| Fold | Description |
|---|---|
| Greater omentum | Apron-like structure that lies superficial to the small intestine and transverse colon; a site of fat deposition in people who are overweight |
| Falciform ligament | Anchors the liver to the anterior abdominal wall and inferior border of the diaphragm |
| Lesser omentum | Suspends the stomach from the inferior border of the liver; provides a pathway for structures connecting to the liver |
| Mesentery | Vertical band of tissue anterior to the lumbar vertebrae and anchoring all of the small intestine except the initial portion (the duodenum) |
| Mesocolon | Attaches two portions of the large intestine (the transverse and sigmoid colon) to the posterior abdominal wall |
The Mouth
The cheeks, tongue, and palate frame the mouth, which is also called the oral cavity (or buccal cavity). The structures of the mouth are illustrated in Figure 13.9.
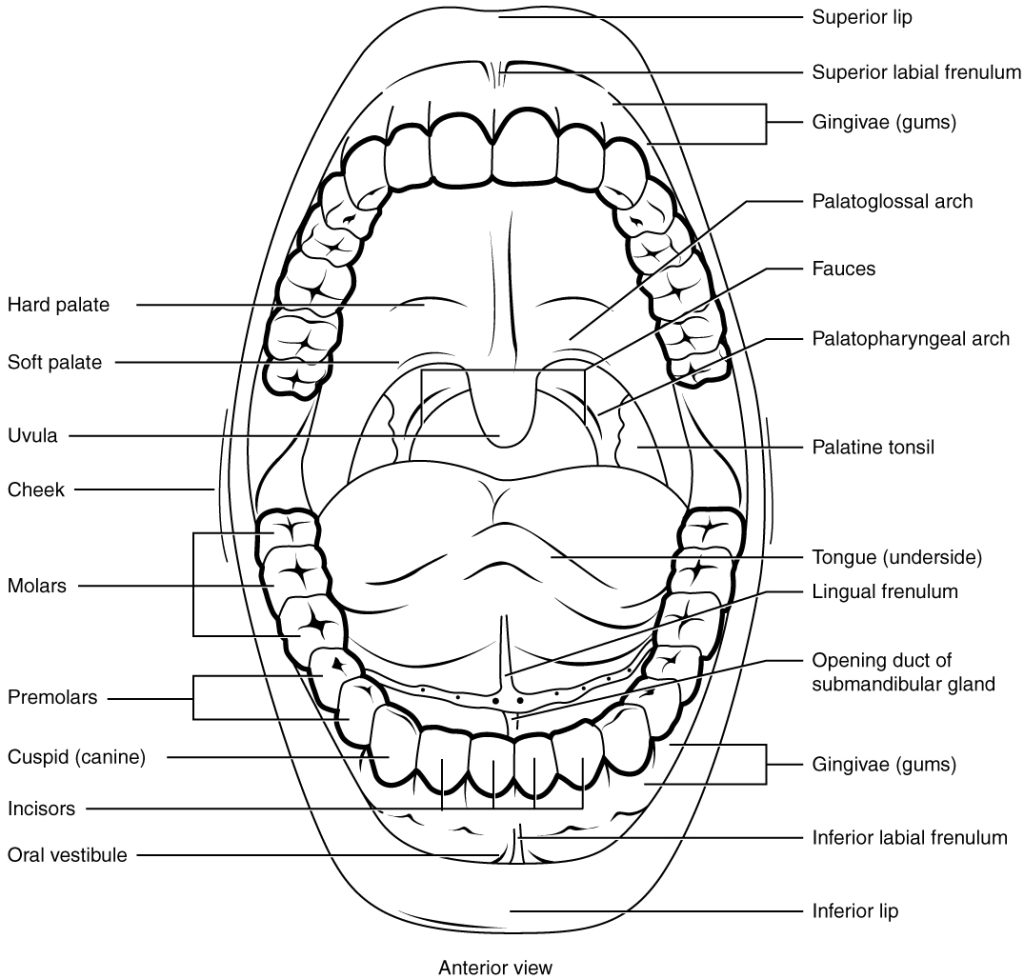
At the entrance to the mouth are the lips, or labia (singular = labium). Their outer covering is skin, which transitions to a mucous membrane in the mouth proper. Lips are very vascular with a thin layer of keratin; hence, the reason they are “red.” The lips cover the orbicularis oris muscle, which regulates what comes in and goes out of the mouth. The labial frenulum is a midline fold of mucous membrane that attaches the inner surface of each lip to the gum. The cheeks make up the oral cavity’s sidewalls. While their outer covering is skin, their inner covering is mucous membrane. This membrane is made up of non-keratinized, stratified squamous epithelium. Between the skin and mucous membranes are connective tissue and buccinator muscles. The next time you eat some food, notice how the buccinator muscles in your cheeks and the orbicularis oris muscle in your lips contract, helping you keep the food from falling out of your mouth. Additionally, notice how these muscles work when you are speaking.
The pocket-like part of the mouth that is framed on the inside by the gums and teeth, and on the outside by the cheeks and lips is called the oral vestibule. Moving farther into the mouth, the opening between the oral cavity and throat (oropharynx) is called the fauces (like the kitchen “faucet”). The main open area of the mouth, or oral cavity proper, runs from the gums and teeth to the fauces.
When you are chewing, you do not find it difficult to breathe simultaneously. The next time you have food in your mouth, notice how the arched shape of the roof of your mouth allows you to handle both digestion and respiration at the same time. This arch is called the palate. The anterior region of the palate serves as a wall (or septum) between the oral and nasal cavities as well as a rigid shelf against which the tongue can push food. It is created by the maxillary and palatine bones of the skull and, given its bony structure, is known as the hard palate. If you run your tongue along the roof of your mouth, you’ll notice that the hard palate ends in the posterior oral cavity, and the tissue becomes fleshier. This part of the palate, known as the soft palate, is composed mainly of skeletal muscle. You can therefore manipulate, subconsciously, the soft palate—for instance, to yawn, swallow, or sing.
A fleshy bead of tissue called the uvula drops down from the center of the posterior edge of the soft palate. Although some have suggested that the uvula is a vestigial organ, it serves an important purpose. When you swallow, the soft palate and uvula move upward, helping to keep foods and liquid from entering the nasal cavity. Unfortunately, it can also contribute to the sound produced by snoring. Two muscular folds extend downward from the soft palate, on either side of the uvula. Toward the front, the palatoglossal arch lies next to the base of the tongue; behind it, the palatopharyngeal arch forms the superior and lateral margins of the fauces. Between these two arches are the palatine tonsils, clusters of lymphoid tissue that protect the pharynx. The lingual tonsils are located at the base of the tongue.
The Tongue
Perhaps you have heard it said that the tongue is the strongest muscle in the body. Those who stake this claim cite its strength proportionate to its size. Although it is difficult to quantify the relative strength of different muscles, it remains indisputable that the tongue is a workhorse, facilitating ingestion, mechanical digestion, chemical digestion (lingual lipase), sensation (of taste, texture, and temperature of food), swallowing, and vocalization.
The tongue is attached to the mandible, the styloid processes of the temporal bones, and the hyoid bone. The tongue is positioned over the floor of the oral cavity. A medial septum extends the entire length of the tongue, dividing it into symmetrical halves.
The Salivary Glands
Many small salivary glands are housed within the mucous membranes of the mouth and tongue. These minor exocrine glands are constantly secreting saliva, either directly into the oral cavity or indirectly through ducts, even while you sleep. In fact, an average of 1 to 1.5 liters of saliva is secreted each day. Usually just enough saliva is present to moisten the mouth and teeth. Secretion increases when you eat, because saliva is essential to moisten food and initiate the chemical breakdown of carbohydrates.
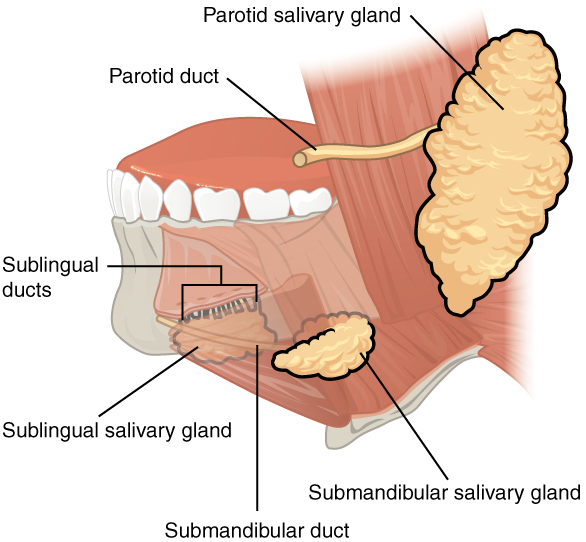
Outside the oral mucosa are three pairs of major salivary glands, which secrete the majority of saliva into ducts that open into the mouth (Figure 13.10):
- The submandibular glands, which are in the floor of the mouth, secrete saliva into the mouth through the submandibular ducts.
- The sublingual glands, which lie below the tongue, use the lesser sublingual ducts to secrete saliva into the oral cavity.
- The parotid glands lie between the skin and the masseter muscle, near the ears. They secrete saliva into the mouth through the parotid duct, which is located near the second upper molar tooth (Figure 13.10).
The Teeth
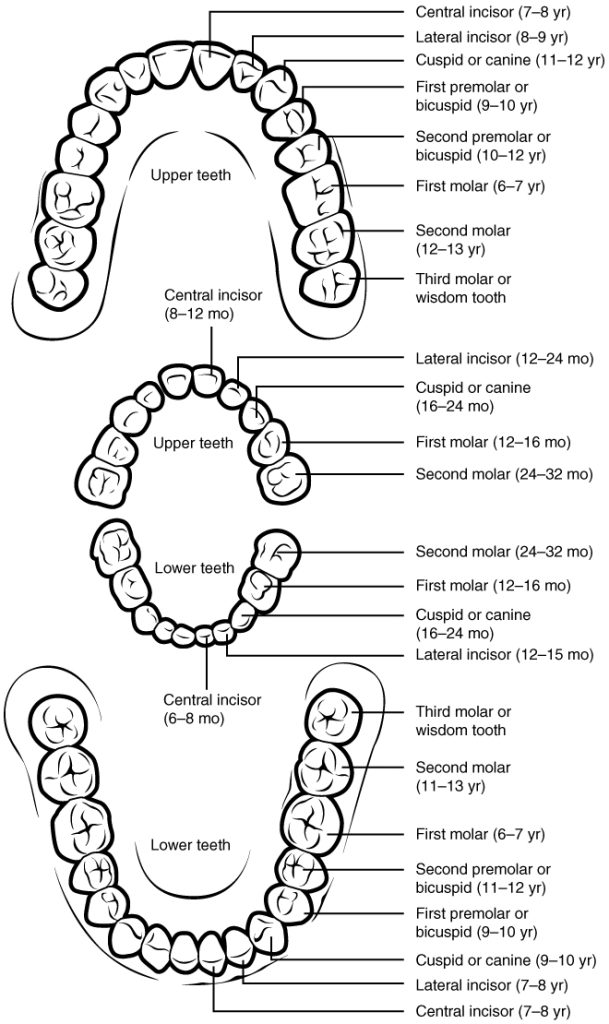
The teeth, or dentes (singular = dens), are organs similar to bones that you use to tear, grind, and otherwise mechanically break down food. During the course of your lifetime, you have two sets of teeth (one set of teeth is a dentition). Your 20 deciduous teeth, or baby teeth, first begin to appear at about 6 months of age. Between approximately age 6 and 12, these teeth are replaced by 32 permanent teeth. Moving from the center of the mouth toward the side, these are as follows (Figure 13.11):
- The eight incisors, four top and four bottom, are the sharp front teeth you use for biting into food.
- The four canines (or cuspids) flank the incisors and have a pointed edge (cusp) to tear up food. These fang-like teeth are superb for piercing tough or fleshy foods.
- Posterior to the cuspids are the eight premolars (or bicuspids), which have an overall flatter shape with two rounded cusps useful for mashing foods.
- The most posterior and largest are the 12 molars, which have several pointed cusps used to crush food so it is ready for swallowing. The third members of each set of three molars, top and bottom, are commonly referred to as the wisdom teeth, because their eruption is commonly delayed until early adulthood. It is not uncommon for wisdom teeth to fail to erupt; that is, they remain impacted. In these cases, the teeth are typically removed by orthodontic surgery.
The teeth are secured in the alveolar processes (sockets) of the maxilla and the mandible. Gingivae (commonly called the gums) are soft tissues that line the alveolar processes and surround the necks of the teeth. Teeth are also held in their sockets by a connective tissue called the periodontal ligament.
The two main parts of a tooth are the crown, which is the portion projecting above the gum line, and the root, which is embedded within the maxilla and mandible. Both parts contain an inner pulp cavity, containing loose connective tissue through which run nerves and blood vessels. The region of the pulp cavity that runs through the root of the tooth is called the root canal. Surrounding the pulp cavity is dentin, a bone-like tissue. In the root of each tooth, the dentin is covered by an even harder bone-like layer called cementum. In the crown of each tooth, the dentin is covered by an outer layer of enamel, the hardest substance in the body (Figure 13.12).
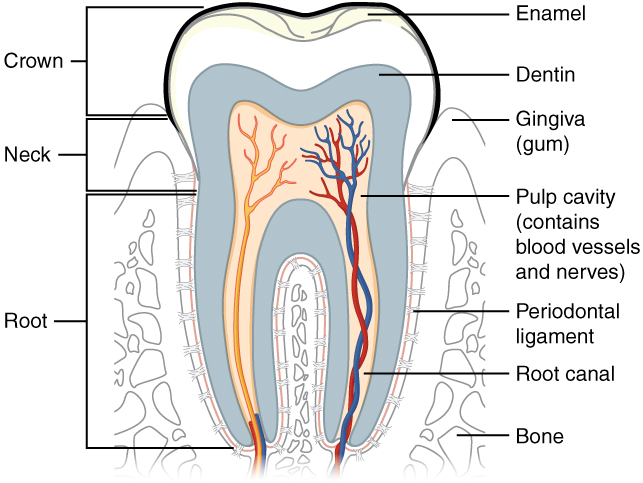
Although enamel protects the underlying dentin and pulp cavity, it is still nonetheless susceptible to mechanical and chemical erosion, or what is known as tooth decay. The most common form, dental caries (cavities) develops when colonies of bacteria feeding on sugars in the mouth release acids that cause soft tissue inflammation and degradation of the calcium crystals of the enamel. The digestive functions of the mouth are summarized in Table 13.4.
The Pharynx
The pharynx (throat) is involved in both digestion and respiration. It receives food and air from the mouth, and air from the nasal cavities. When food enters the pharynx, involuntary muscle contractions close off the air passageways.
A short tube of skeletal muscle lined with a mucous membrane, the pharynx runs from the posterior oral and nasal cavities to the opening of the esophagus and larynx. It has three subdivisions. The most superior, the nasopharynx, is involved only in breathing and speech. The other two subdivisions, the oropharynx and the laryngopharynx, are used for both breathing and digestion. The oropharynx begins inferior to the nasopharynx and is continuous below with the laryngopharynx (Figure 13.13). The inferior border of the laryngopharynx connects to the esophagus, whereas the anterior portion connects to the larynx, allowing air to flow into the bronchial tree.
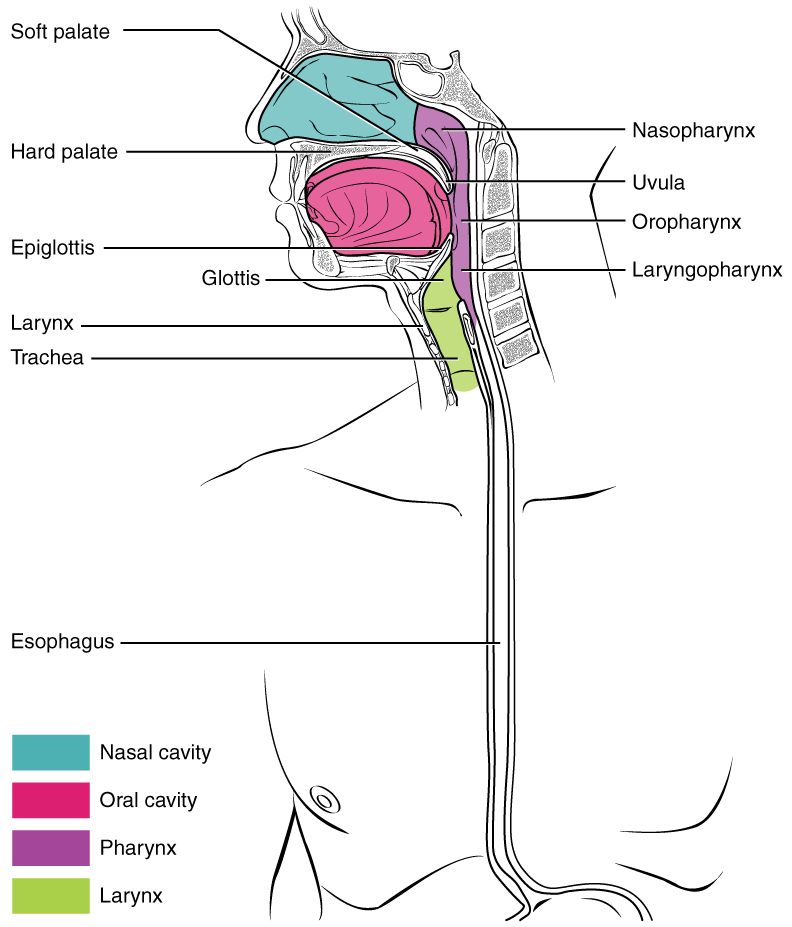
Histologically, the wall of the oropharynx is similar to that of the oral cavity. The mucosa includes a stratified squamous epithelium that is endowed with mucus-producing glands. During swallowing, the elevator skeletal muscles of the pharynx contract, raising and expanding the pharynx to receive the bolus of food. Once received, these muscles relax and the constrictor muscles of the pharynx contract, forcing the bolus into the esophagus and initiating peristalsis.
Usually during swallowing, the soft palate and uvula rise reflexively to close off the entrance to the nasopharynx. At the same time, the larynx is pulled superiorly and the cartilaginous epiglottis, its most superior structure, folds inferiorly, covering the glottis (the opening to the larynx); this process effectively blocks access to the trachea and bronchi. When the food “goes down the wrong way,” it goes into the trachea. When food enters the trachea, the reaction is to cough, which usually forces the food up and out of the trachea, and back into the pharynx.
The Esophagus
The esophagus is a muscular tube that connects the pharynx to the stomach. It is approximately 25.4 cm (10 in) in length, located posterior to the trachea, and remains in a collapsed form when not engaged in swallowing. The esophagus runs a mainly straight route through the mediastinum of the thorax. To enter the abdomen, the esophagus penetrates the diaphragm through an opening called the esophageal hiatus.
The mucosa of the esophagus is made up of an epithelial lining that contains non-keratinized, stratified squamous epithelium. This epithelium protects against erosion from food particles. The mucosa’s lamina propria contains mucus-secreting glands. The muscularis layer changes according to location: In the upper third of the esophagus, the muscularis is skeletal muscle. In the middle third, it is both skeletal and smooth muscle. In the lower third, it is smooth muscle. As mentioned previously, the most superficial layer of the esophagus is called the adventitia, not the serosa. In contrast to the stomach and intestines, the loose connective tissue of the adventitia is not covered by a fold of visceral peritoneum.
The Stomach
Although a minimal amount of carbohydrate digestion occurs in the mouth, chemical digestion really gets underway in the stomach. An expansion of the alimentary canal that lies immediately inferior to the esophagus, the stomach links the esophagus to the first part of the small intestine (the duodenum) and is relatively fixed in place at its esophageal and duodenal ends. In between, however, it can be a highly active structure, contracting and continually changing position and size. These contractions provide mechanical assistance to digestion. The empty stomach is only about the size of your fist, but can stretch to hold as much as 4 liters of food and fluid, or more than 75 times its empty volume, and then return to its resting size when empty.
Popular culture tends to refer to the stomach as the location where all digestion takes place. Of course, this is not true. An important function of the stomach is to serve as a temporary holding chamber. You can ingest a meal far more quickly than it can be digested and absorbed by the small intestine. Thus, the stomach holds food and parses only small amounts into the small intestine at a time. Before food is released to the small intestine, it is mixed together with digestive juices in the stomach and converted into chyme. The stomach plays several important roles in chemical digestion, including the continued digestion of carbohydrates and the initial digestion of proteins and triglycerides. Little if any nutrient absorption occurs in the stomach, with the exception of the negligible amount of nutrients in alcohol.
There are four main regions in the stomach: the cardia, fundus, body, and pylorus (Figure 13.14). The cardia (or cardiac region) is the point where the esophagus connects to the stomach and through which food passes into the stomach. Located inferior to the diaphragm, above and to the left of the cardia, is the dome-shaped fundus. Below the fundus is the body, the main part of the stomach. The funnel-shaped pylorus connects the stomach to the duodenum. The wider end of the funnel, the pyloric antrum, connects to the body of the stomach. The narrower end is called the pyloric canal, which connects to the duodenum. The smooth muscle pyloric sphincter is located at this latter point of connection and controls stomach emptying. In the absence of food, the stomach deflates inward, and its mucosa and submucosa fall into a large fold called a ruga.
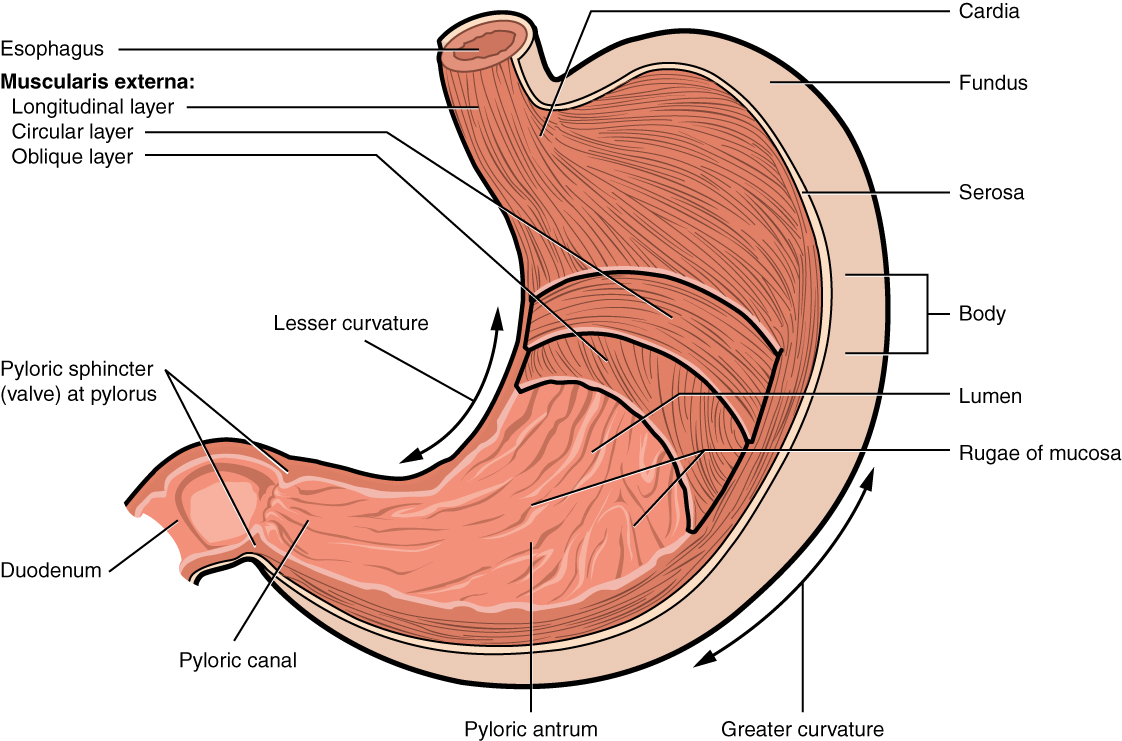
The convex lateral surface of the stomach is called the greater curvature; the concave medial border is the lesser curvature. The stomach is held in place by the lesser omentum, which extends from the liver to the lesser curvature, and the greater omentum, which runs from the greater curvature to the posterior abdominal wall.
The Small Intestine
Chyme released from the stomach enters the small intestine, which is the primary digestive organ in the body. Not only is this where most digestion occurs, it is also where practically all absorption occurs. The longest part of the alimentary canal, the small intestine is about 3.05 meters (10 feet) long in a living person (but about twice as long in a cadaver due to the loss of muscle tone). Since this makes it about five times longer than the large intestine, you might wonder why it is called “small.” In fact, its name derives from its relatively smaller diameter of only about 2.54 cm (1 in), compared with 7.62 cm (3 in) for the large intestine. As we’ll see shortly, in addition to its length, the folds and projections of the lining of the small intestine work to give it an enormous surface area, which is approximately 200 m2, more than 100 times the surface area of your skin. This large surface area is necessary for complex processes of digestion and absorption that occur within it.
The coiled tube of the small intestine is subdivided into three regions. From proximal (at the stomach) to distal, these are the duodenum, jejunum, and ileum (Figure 13.15). The shortest region is the 25.4-cm (10-in) duodenum, which begins at the pyloric sphincter. Just past the pyloric sphincter, it bends posteriorly behind the peritoneum, becoming retroperitoneal, and then makes a C-shaped curve around the head of the pancreas before ascending anteriorly again to return to the peritoneal cavity and join the jejunum. Of particular interest is the hepatopancreatic ampulla. Located in the duodenal wall, the ampulla marks the transition from the anterior portion of the alimentary canal to the mid-region, and is where the bile duct (through which bile passes from the liver) and the main pancreatic duct (through which pancreatic juice passes from the pancreas) join. This ampulla opens into the duodenum at a tiny volcano-shaped structure called the major duodenal papilla. The hepatopancreatic sphincter regulates the flow of both bile and pancreatic juice from the ampulla into the duodenum.
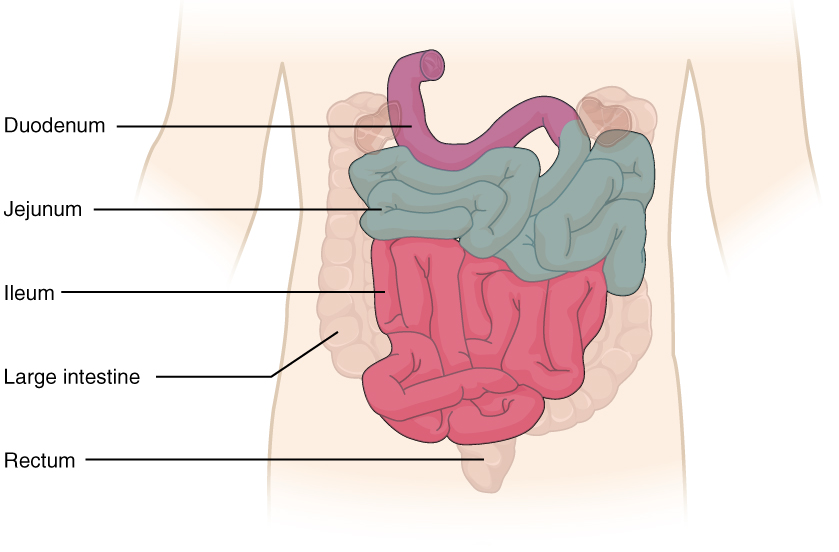
The jejunum is about 0.9 meters (3 feet) long (in life) and runs from the duodenum to the ileum. Jejunum means “empty” in Latin and supposedly was so named by the ancient Greeks who noticed it was always empty at death. No clear demarcation exists between the jejunum and the final segment of the small intestine, the ileum. The ileum is the longest part of the small intestine, measuring about 1.8 meters (6 feet) in length. It is thicker, more vascular, and has more developed mucosal folds than the jejunum. The ileum joins the cecum, the first portion of the large intestine, at the ileocecal valve (or sphincter). The jejunum and ileum are tethered to the posterior abdominal wall by the mesentery. The large intestine frames these three parts of the small intestine.
Histology of the small intestine
The wall of the small intestine is composed of the same four layers typically present in the alimentary system. However, three features of the mucosa and submucosa are unique. These features, which increase the absorptive surface area of the small intestine more than 600-fold, include circular folds, villi, and microvilli (Figure 13.16). These adaptations are most abundant in the proximal two-thirds of the small intestine, where the majority of absorption occurs.
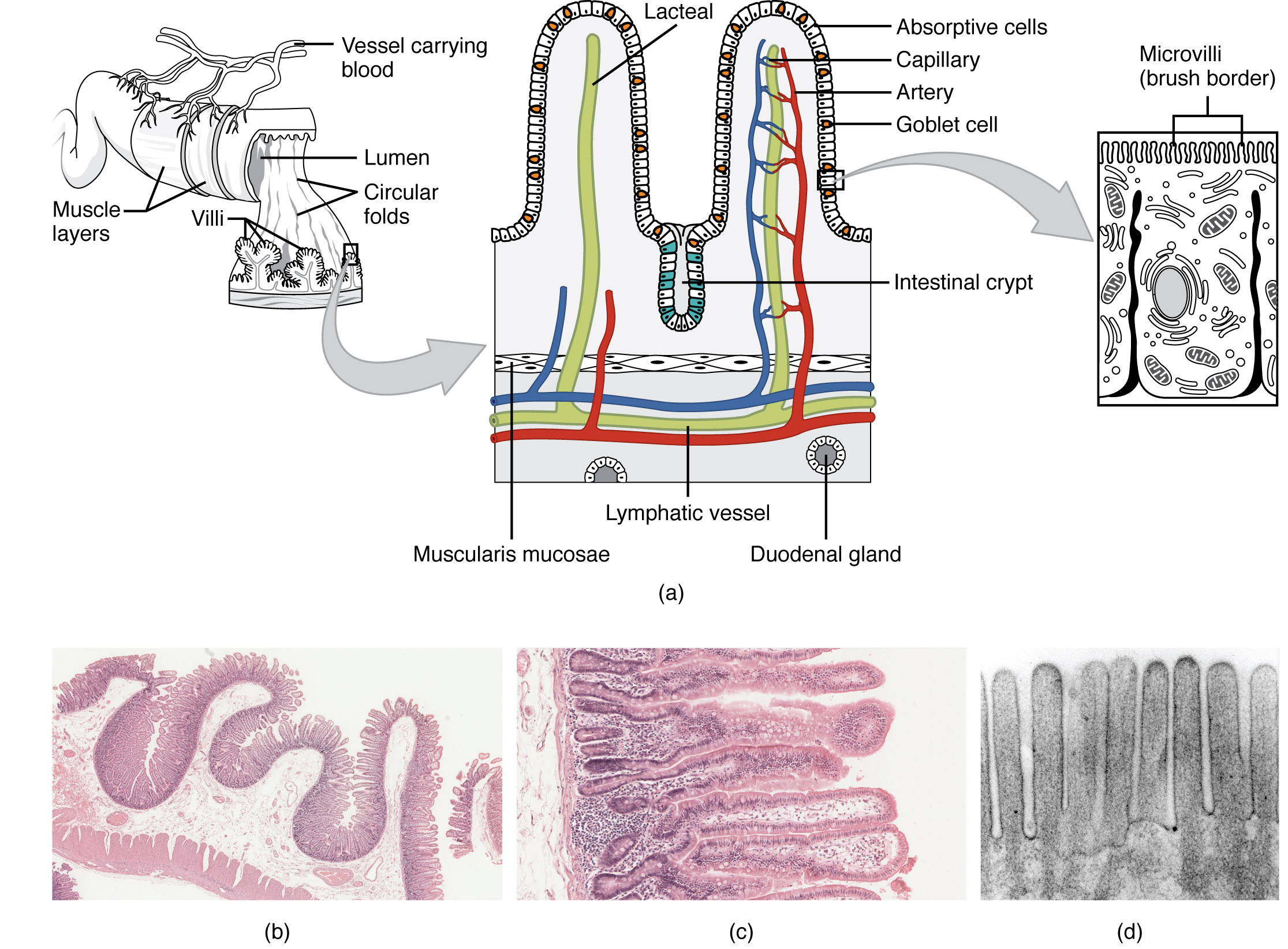
Also called a plica circulare, a circular fold is a deep ridge in the mucosa and submucosa. Beginning near the proximal part of the duodenum and ending near the middle of the ileum, these folds facilitate absorption. Their shape causes the chyme to spiral, rather than move in a straight line, through the small intestine. Spiraling slows the movement of chyme and provides the time needed for nutrients to be fully absorbed.
Within the circular folds are small (0.5–1 mm long) hairlike vascularized projections called villi (singular = villus) that give the mucosa a furry texture. There are about 20 to 40 villi per square millimeter, increasing the surface area of the epithelium tremendously. The mucosal epithelium, primarily composed of absorptive cells, covers the villi. In addition to muscle and connective tissue to support its structure, each villus contains a capillary bed composed of one arteriole and one venule, as well as a lymphatic capillary called a lacteal. The breakdown products of carbohydrates and proteins (sugars and amino acids) can enter the bloodstream directly, but lipid breakdown products are absorbed by the lacteals and transported to the bloodstream via the lymphatic system.
As their name suggests, microvilli (singular = microvillus) are much smaller (1 µm) than villi. They are cylindrical apical surface extensions of the plasma membrane of the mucosa’s epithelial cells. Although their small size makes it difficult to see each microvillus, their combined microscopic appearance suggests a mass of bristles, which is termed the brush border. There are an estimated 200 million microvilli per square millimeter of small intestine, greatly expanding the surface area of the plasma membrane and thus greatly enhancing absorption.
Chemical Digestion in the Small Intestine
The digestion of proteins and carbohydrates, which partially occurs in the stomach, is completed in the small intestine with the aid of intestinal and pancreatic juices. Lipids arrive in the intestine largely undigested, so much of the focus here is on lipid digestion, which is facilitated by bile and the enzyme pancreatic lipase. Intestinal juice combines with pancreatic juice to provide a liquid medium that facilitates absorption. The intestine is also where most water is absorbed, via osmosis.
For optimal chemical digestion, chyme must be delivered from the stomach slowly and in small amounts. This is because chyme from the stomach is typically hypertonic, and if large quantities were forced all at once into the small intestine, the resulting osmotic water loss from the blood into the intestinal lumen would result in potentially life-threatening low blood volume. In addition, continued digestion requires an upward adjustment of the low pH of stomach chyme, along with rigorous mixing of the chyme with bile and pancreatic juices. Both processes take time, so the pumping action of the pylorus must be carefully controlled to prevent the duodenum from being overwhelmed with chyme.
The Large Intestine
The large intestine is the terminal part of the alimentary canal. The primary function of this organ is to finish absorption of nutrients and water, synthesize certain vitamins, form feces, and eliminate feces from the body. The small intestine absorbs about 90 percent of the water you ingest (either as liquid or within solid food). The large intestine absorbs most of the remaining water, a process that converts the liquid chyme residue into semisolid feces (“stool”).
The large intestine runs from the appendix to the anus. It frames the small intestine on three sides. Despite its being about one-half as long as the small intestine, it is called large because it is more than twice the diameter of the small intestine, about 3 inches. The large intestine is subdivided into four main regions: the cecum, the colon, the rectum, and the anus. The ileocecal valve, located at the opening between the ileum and the large intestine, controls the flow of chyme from the small intestine to the large intestine.
The first part of the large intestine is the cecum, a sac-like structure that is suspended inferior to the ileocecal valve. It is about 6 cm (2.4 in) long, receives the contents of the ileum, and continues the absorption of water and salts. The appendix (or vermiform appendix) is a winding tube that attaches to the cecum. Although the 7.6-cm (3-in) long appendix contains lymphoid tissue, suggesting an immunologic function, this organ is generally considered vestigial.
The cecum blends seamlessly with the colon. Upon entering the colon, the food residue first travels up the ascending colon on the right side of the abdomen. At the inferior surface of the liver, the colon bends to form the right colic flexure (hepatic flexure) and becomes the transverse colon. Food residue passing through the transverse colon travels across to the left side of the abdomen, where the colon angles sharply immediately inferior to the spleen, at the left colic flexure (splenic flexure). From there, food residue passes through the descending colon, which runs down the left side of the posterior abdominal wall. After entering the pelvis inferiorly, it becomes the s-shaped sigmoid colon, which extends medially to the midline (Figure 13.17). The ascending and descending colon, and the rectum are located in the retroperitoneum. The transverse and sigmoid colon are tethered to the posterior abdominal wall by the mesocolon.
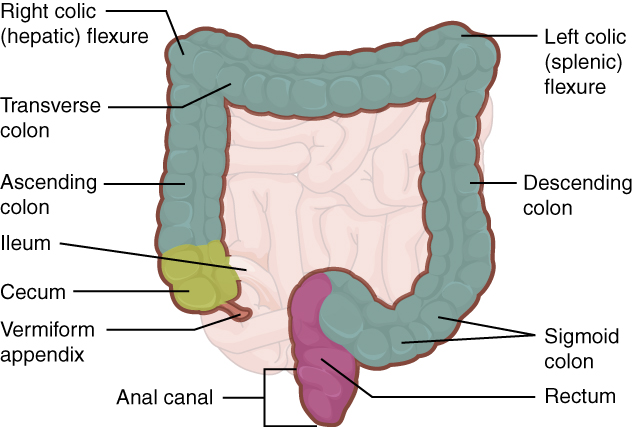
Food residue leaving the sigmoid colon enters the rectum in the pelvis, near the third sacral vertebra. The final 20.3 cm (8 in) of the alimentary canal, the rectum extends anterior to the sacrum and coccyx. Even though rectum is Latin for “straight,” this structure follows the curved contour of the sacrum and has three lateral bends that create a trio of internal transverse folds called the rectal valves. These valves help separate the feces from gas to prevent the simultaneous passage of feces and gas.
Finally, food residue reaches the last part of the large intestine, the anal canal, which is located in the perineum, completely outside of the abdominopelvic cavity. This 3.8–5 cm (1.5–2 in) long structure opens to the exterior of the body at the anus. The anal canal includes two sphincters. The internal anal sphincter is made of smooth muscle, and its contractions are involuntary. The external anal sphincter is made of skeletal muscle, which is under voluntary control. Except when defecating, both usually remain closed.
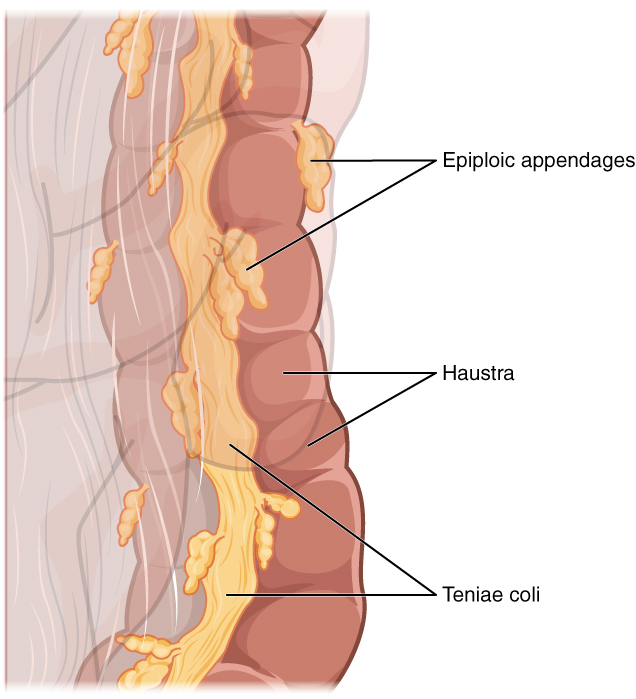
Three features are unique to the large intestine: teniae coli, haustra, and epiploic appendages (Figure 13.18). The teniae coli are three bands of smooth muscle that make up the longitudinal muscle layer of the muscularis of the large intestine, except at its terminal end. Tonic contractions of the teniae coli bunch up the colon into a succession of pouches called haustra (singular = haustrum), which are responsible for the wrinkled appearance of the colon. Attached to the teniae coli are small, fat-filled sacs of visceral peritoneum called epiploic appendages. The purpose of these is unknown. Although the rectum and anal canal have neither teniae coli nor haustra, they do have well-developed layers of muscularis that create the strong contractions needed for defecation.
Accessory Organs of the Digestive System
Chemical digestion in the small intestine relies on the activities of three accessory digestive organs: the liver, pancreas, and gallbladder (Figure 13.19). The digestive role of the liver is to produce bile and export it to the duodenum. The gallbladder primarily stores, concentrates, and releases bile. The pancreas produces pancreatic juice, which contains digestive enzymes and bicarbonate ions, and delivers it to the duodenum.
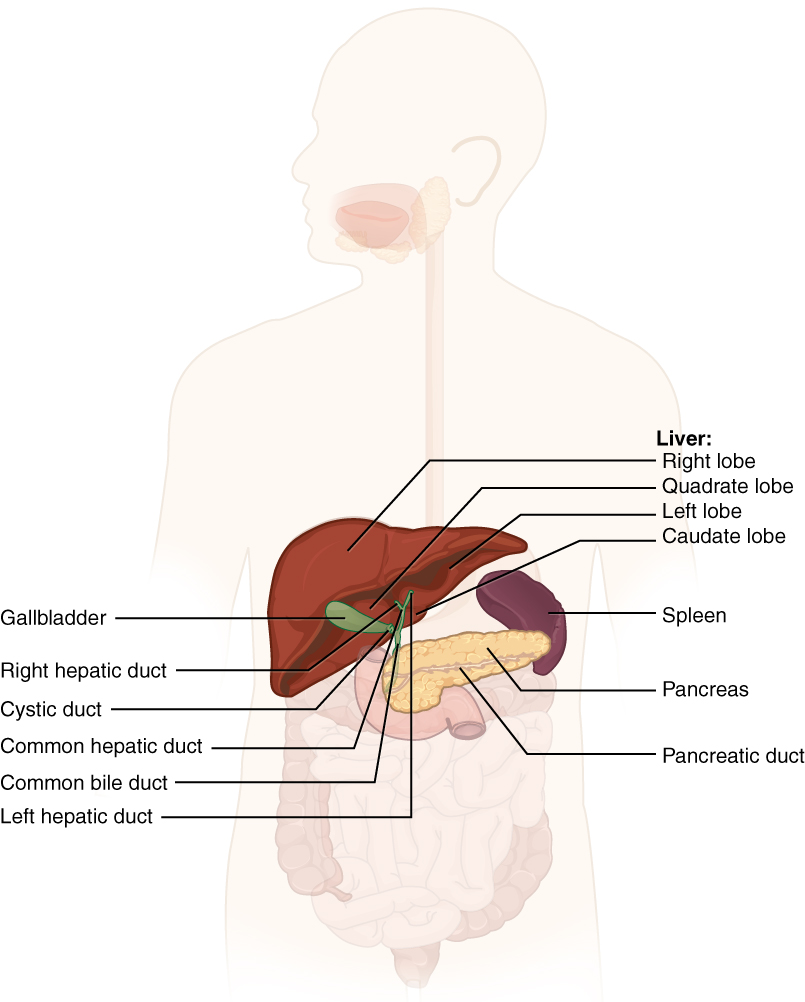
The Liver
The liver is the largest gland in the body, weighing about three pounds in an adult. It is also one of the most important organs. In addition to being an accessory digestive organ, it plays a number of roles in metabolism and regulation. The liver lies inferior to the diaphragm in the right upper quadrant of the abdominal cavity and receives protection from the surrounding ribs.
The liver is divided into two primary lobes: a large right lobe and a much smaller left lobe. In the right lobe, some anatomists also identify an inferior quadrate lobe and a posterior caudate lobe, which are defined by internal features. The liver is connected to the abdominal wall and diaphragm by five peritoneal folds referred to as ligaments. These are the falciform ligament, the coronary ligament, two lateral ligaments, and the ligamentum teres hepatis. The falciform ligament and ligamentum teres hepatis are actually remnants of the umbilical vein, and separate the right and left lobes anteriorly. The lesser omentum tethers the liver to the lesser curvature of the stomach.
The porta hepatis (“gate to the liver”) is where the hepatic artery and hepatic portal vein enter the liver. These two vessels, along with the common hepatic duct, run behind the lateral border of the lesser omentum on the way to their destinations. The hepatic artery delivers oxygenated blood from the heart to the liver. The hepatic portal vein delivers partially deoxygenated blood containing nutrients absorbed from the small intestine and actually supplies more oxygen to the liver than do the much smaller hepatic arteries. In addition to nutrients, drugs and toxins are also absorbed. After processing the bloodborne nutrients and toxins, the liver releases nutrients needed by other cells back into the blood, which drains into the central vein and then through the hepatic vein to the inferior vena cava. With this hepatic portal circulation, all blood from the alimentary canal passes through the liver. This largely explains why the liver is the most common site for the metastasis of cancers that originate in the alimentary canal.
The common hepatic duct transports bile from the liver (coming from the left and right hepatic ducts) towards the small intestine. Bile is a mixture secreted by the liver to accomplish the emulsification of lipids in the small intestine. Recall that lipids are hydrophobic, that is, they do not dissolve in water. Thus, before they can be digested in the watery environment of the small intestine, large lipid globules must be broken down into smaller lipid globules, a process called emulsification. Hepatocytes secrete about one liter of bile each day. Hepatocytes work non-stop, but bile production increases when fatty chyme enters the duodenum and stimulates the secretion of the gut hormone secretin. Between meals, bile is produced but conserved. The valve-like hepatopancreatic ampulla closes, allowing bile to divert to the gallbladder, where it is concentrated and stored until the next meal.
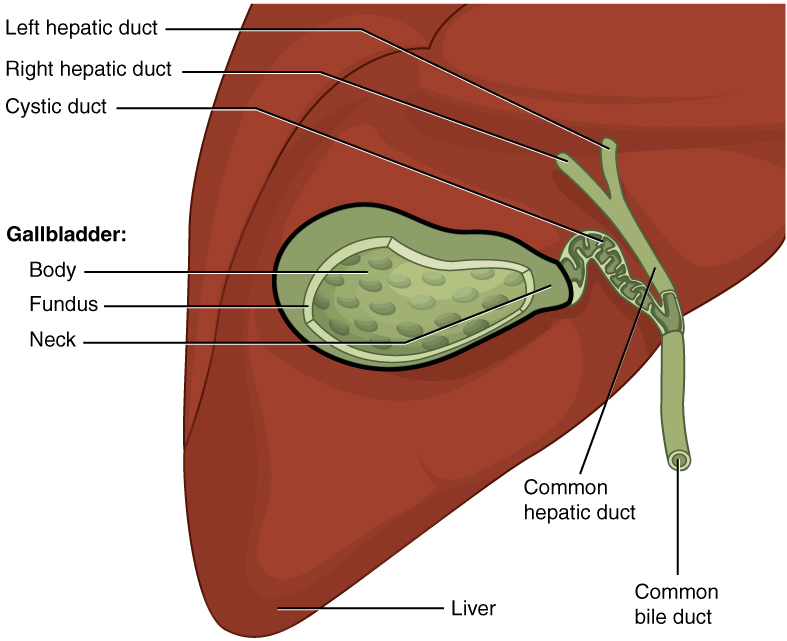
The Gallbladder
The gallbladder is 8–10 cm (~3–4 in) long and is nested in a shallow area on the posterior aspect of the right lobe of the liver. This muscular sac stores, concentrates, and, when stimulated, propels the bile into the duodenum via the common bile duct. It is divided into three regions. The fundus is the widest portion and tapers medially into the body, which in turn narrows to become the neck. The neck angles slightly superiorly as it approaches the hepatic duct. The cystic duct is 1–2 cm (less than 1 in) long and turns inferiorly as it bridges the neck and hepatic duct.
The simple columnar epithelium of the gallbladder mucosa is organized in rugae, similar to those of the stomach. The gallbladder has a layer of smooth muscle fibers, which, when they contract, eject the gallbladder’s contents through the cystic duct and into the common bile duct (Figure 13.20). Visceral peritoneum reflected from the liver capsule holds the gallbladder against the liver and forms the outer coat of the gallbladder. The gallbladder’s mucosa absorbs water and ions from bile, concentrating it by up to 10-fold.
The Pancreas
The soft, oblong, glandular pancreas lies transversely in the retroperitoneum behind the stomach. Its head is nestled into the “c-shaped” curvature of the duodenum with the body extending to the left about 15.2 cm (6 in) and ending as a tapering tail in the hilum of the spleen (Figure 13.21). It is a curious mix of exocrine (secreting digestive enzymes) and endocrine (releasing hormones into the blood) functions.
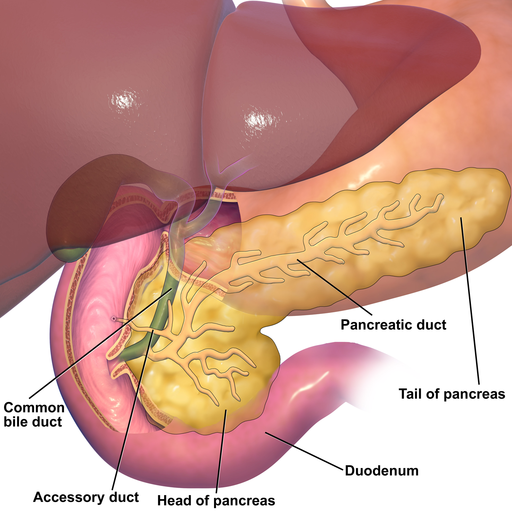
The exocrine part of the pancreas arises as little grape-like cell clusters, each called an acinus (plural = acini), located at the terminal ends of pancreatic ducts. These acinar cells secrete enzyme-rich pancreatic juice into tiny merging ducts that form two dominant ducts. The larger pancreatic duct fuses with the common bile duct (carrying bile from the liver and gallbladder) just before entering the duodenum via a common opening (the hepatopancreatic ampulla). The smooth muscle sphincter of the hepatopancreatic ampulla controls the release of pancreatic juice and bile into the small intestine. The second and smaller pancreatic duct, the accessory duct, runs from the pancreas directly into the duodenum, approximately 1 inch above the hepatopancreatic ampulla.
The pancreas produces over a liter of pancreatic juice each day. Unlike bile, it is clear and composed mostly of water along with some salts, sodium bicarbonate, and several digestive enzymes. Sodium bicarbonate is responsible for the slight alkalinity of pancreatic juice (pH 7.1 to 8.2), which serves to buffer the acidic gastric juice in chyme, inactivate pepsin from the stomach, and create an optimal environment for the activity of pH-sensitive digestive enzymes in the small intestine. Pancreatic enzymes are active in the digestion of sugars, proteins, and fats.
Unless otherwise indicated, this chapter contains material adapted from chapters 17 and 23 in Anatomy and Physiology (on OpenStax), by Betts, et al. and is used under a a CC BY 4.0 international license. Download and access OpenStax Anatomy and Physiology for free at https://openstax.org/books/anatomy-and-physiology-2e/

