Gametogenesis, Fertilization, and Implantation
Implantation
Implantation occurs when the conceptus adheres to the wall of the uterus, signaling the end of the pre-embryonic stage of development.
As the zona pellucida begins to fragment, the blastocyst is able to attach to the uterine endometrium. By this time, progesterone and estrogen produced by the corpus luteum lead to the proper proliferation and differentiation of the endometrium. As the endometrium continues its maturation, a decidua layer is formed. The maturation of the endometrium and formation of a secretory endometrium is called decidualization. Around the end of the first week, the blastocyst comes into contact with the secretory uterine wall and adheres to it, embedding itself in the uterine lining via the trophoblast cells. Thus begins the process of implantation.
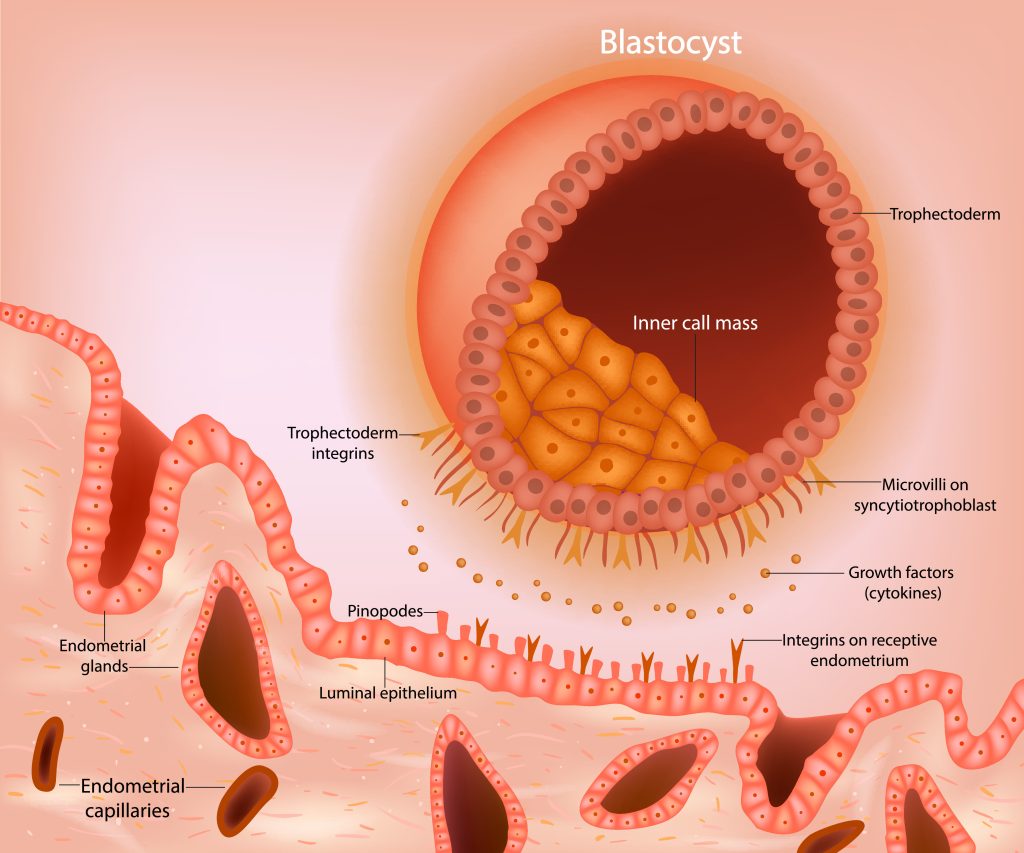
The inner cell layer of the trophoblast of the blastocyst, called the cytotrophoblast, forms the fetal surface of the placenta. The outer layer of the trophoblast, known as the syncytiotrophoblast, contributes to the maternal surface of placenta that fuses with endometrial cells. The syncytiotrophoblast cells lose their cell walls and become the working interface of the placenta. The cytoplasm of the cells fuse and form a multinucleated cytoplasm. Then, the syncytiotrophoblast layer invaginates into the decidua and is surrounded by lakes of maternal blood, allowing the efficient transfer of oxygen, nutrients, and waste products bidirectionally without the direct mixing of maternal and fetal blood.
The syncytiotrophoblast cells produce human chorionic gonadotropin (hCG), a hormone that directs the corpus luteum to survive, enlarge, and continue producing progesterone and estrogen to suppress menses. These functions of hCG are necessary for creating an environment suitable for the developing embryo. As a result of this increased production, hCG accumulates in the maternal bloodstream and is excreted in the urine. Implantation is complete by the middle of the second week. Just a few days after implantation, the trophoblast has secreted enough hCG for an at-home urine pregnancy test to give a positive result. hCG is the marker used for mass pregnancy tests.
Implantation can be accompanied by minor bleeding. The blastocyst typically implants in the fundus of the uterus or on the posterior wall. However, if the endometrium is not fully developed and is not ready to receive the blastocyst, the blastocyst will detach and find a better spot. A significant percentage (50–75 percent) of blastocysts fail to implant; when this occurs, the blastocyst is shed with the endometrium during menses. The high rate of implantation failure is one reason why pregnancy typically requires several ovulation cycles to achieve.
Clinical Correlation
Precise timing of endometrial lining and implantation
The time from ovulation to implantation takes approximately 10–12 days. Proper timing for the arrival of the conceptus into the uterine cavity is essential for implantation. During IVF techniques, the maturation of the endometrium must be coordinated precisely with the developmental stage of the conceptus transferred into the uterus for optimal pregnancy rates. Attempts at tubal re-anastomosis may be followed by too short of the oviduct (<4cm). Short tubes might accelerate the transport of the conceptus through the tubes and diminish pregnancy rates.
Take Home Message
- Trophoblast cells produce hCG, the marker ised for mass pregnancy tests.
- A positive pregnancy test is an indication that implantation has occurred.
Image Sources
- Figure 1. “Blastocyst implantation” by sakurra was licensed through Adobe Stock for educational use.

