Genetic Disorders
Prenatal Diagnosis and Genetic Counseling
Prenatal diagnosis and genetic counseling usually help detect genetic disorders and birth defects before the third trimester. This early diagnosis gives the parent the option to terminate their pregnancy early if necessary, or at the very least, the time to emotionally acclimate to the situation. It also improves the management of pregnancy, delivery, and the neonatal period accordingly.
Methods and procedures for prenatal diagnosis
Genetic History
Obtaining and documenting a thorough genetic history alone is important. It can help narrow done and possibly rule out chances of a genetic order or birth defect. Health status and history of first-, second-, and third-degree relatives will be gathered. Any history of repetitive spontaneous miscarriage, stillbirths, and anomalous fetuses will be recorded. The ethnicities, ages, and any drug exposure of the mother and father will also be recorded.
Fetal Ultrasound
Fetal ultrasounds are a harmless process to the fetus and mother. It is important to have ultrasounds of the fetus taken during the pregnancy, as this gives the doctors the ability to analyze the developmental progress of the fetus. At 5 weeks post-conception, a vaginal probe can be performed. At 12 weeks post-conception an abdominal ultrasound can be performed. A fetal ultrasound could detect fetal size, growth, number of fetuses, viability, and amniotic fluid volume. Ultrasounds done at centers specialized in the care of high-risk pregnancies can also help detect structural abnormalities in the many organs.
Maternal Serum Alpha Fetoprotein (AFP)
Maternal serum alpha fetoprotein (MSAFP) levels can be tested at 15 to 17 weeks of gestation. A low level of MSAFP is indicative of an increased risk of trisomy in the fetus. A high level of MSAFP is indicative of a risk for open defects of the neural tube or GI tract.
Genetic Amniocentesis
Genetic amniocentesis is a procedure that involves puncturing the amniotic sac with a needle to gather a sample of fetal cells from the amniotic fluid. This procedure can be performed from 16 to 18 weeks of gestation via the withdrawal of about 30 mL of amniotic fluid. The fetal cells gathered can be used for fetal DNA analysis and fetal karyotype. A pregnant woman should be offered this option if she meets the following criteria: 35 years or older, history of multiple miscarriages, family history of genetic disease, or abnormal levels of MSAFP detected.
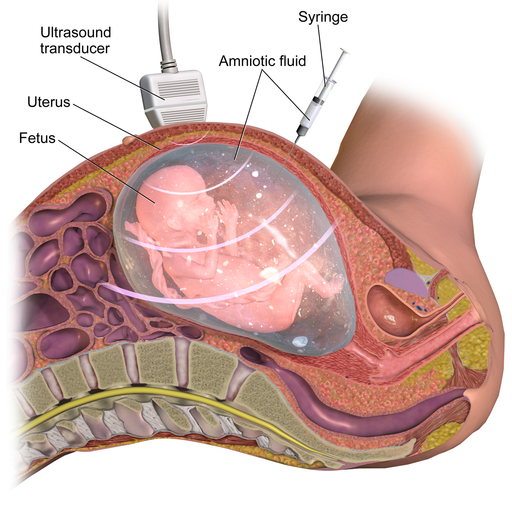
Amniocentesis is an invasive and high-risk procedure. It may lead to the leakage of amniotic fluid, spontaneous labor, or puncture of the fetus. The incidence of spontaneous abortion may result in approximately 1/200 to 1/400 of cases after amniocentesis.
Chorionic Villi Sampling (CVS)
Chorionic villi sampling (CVS) involves either a catheter being inserted into the cervix guided by a trans-vaginal ultrasound, or a needle inserted trans-abdominally into the placenta to aspirate chorionic villi cells from the placenta. CVS can be performed from 9 to 12 weeks of gestation, but it is associated with a 1% risk of fetal loss. The aspirated cells can be used for fetal DNA analysis and fetal karyotype; however, the results may be ambiguous.
Percutaneous Umbilical Cord Blood Sampling (PUBS)
Percutaneous umbilical cord blood sampling (PUBS) is a procedure involving an ultrasound-guided needle which is punctured into the fetal umbilical blood vessels to get a sample of fetal blood. This fetal blood sample can be used for fetal DNA analysis, fetal karyotype, fetal blood count, or assessment of the fetal acid base status. This procedure can be done at 18 weeks of gestation, but has a fairly high risk of fetal loss at 2-3%.
Genetic Council and Termination of Pregnancy
There are many different genetic disorders to look out for when it comes to pregnancy. It is very important for a pregnant woman or even a woman thinking of getting pregnant to get genetic counseling as well as prenatal diagnosis when necessary. This empowers the prospective parents to make informed decisions if a genetic disorder is identified, including whether to continue or terminate the pregnancy.
It is important to recognize that there are legal regulations in place governing an individual’s choice to terminate a pregnancy at different stages of gestation. During the first trimester, the decision to terminate lies entirely with the pregnant woman and her physician. During the second trimester, there may be state regulations imposed with respect to the mother’s health. During the third trimester, abortion may be regulated by the state unless the mother’s health is of concern.
These regulations highlight the significance of early diagnosis in pregnancy, allowing sufficient time for thoughtful decision-making, taking into account both medical and legal considerations.
Take Home Message
- Ultrasounds are a safe and easy method to detect fetal anomalies.
- CVS has the highest risk of losing a fetus during prenatal diagnosis of congenital malformation.
Image Sources
- Figure 1. “Amniocentesis” is from Bruce Blaus via Wikimedia, licensed CC BY SA 4.0.

