Stages of Life
Menopause
Menopause is a permanent cessation of menses because of a loss of ovarian activity, usually identified retrospectively when an older female has not had a period for over a year. The age of menopause varies depending on various inherited and environmental factors. The average age of menopause in American women is 51 (range 48-55 years). If menopause happens before the age of 40, that is considered premature menopause. Some factors like cigarette smoking, living at high altitudes, exposure to some chemotherapeutic agents, or hysterectomy tend to slightly lower the age of menopause and cause the final cessation of ovulation leading to early menopause.
Perimenopause
Perimenopause is the time just before and after menopause, around the age of 45-55 years. This time is considered a transition to menopause. It is associated with the early onset of symptoms like mood swings, vasomotor flushes, sleep disturbances, headaches, memory problems, decreased libido, urinary incontinence, and irregular cycles. It is accompanied by fluctuations in ovarian function, decreased number and maturation of the remaining follicles, and decreased sensitivity to gonadotropin. Fertility rates are markedly reduced, but conception can occur, as exhaustion of all follicles is not complete yet.
Hormonal changes at menopause
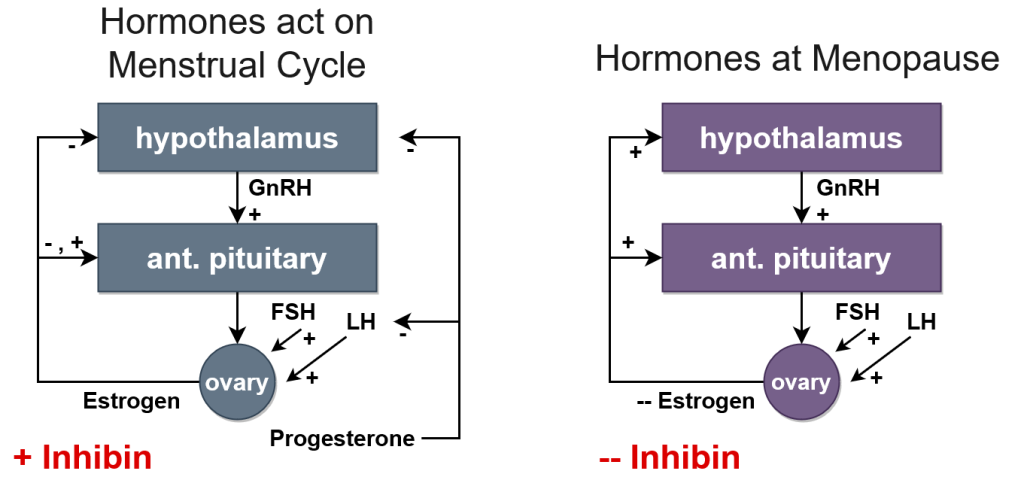
During the transition from menses to menopause, there are some hormonal changes due to the decrease in ovarian cells’ sensitivity to gonadotropin stimulation, exhaustion of the supply of ovarian follicles, and loss of ovarian cells that secrete estrogen and progesterone. As a result, estrogen and inhibin levels are reduced. Decreased estrogen and inhibin remove the negative feedback on the higher centers. As the negative feedback is removed, gonadotropin, FSH, and LHs level are increased (Figure 1). A state of hypergonadotropic-amenorrhea develops among menopausal women.
Effects of Estrogen Deficiency
The deficiency of estrogen can cause many physical complaints and changes in menopausal women, which include:
Vasomotor Instability
The most common complaint, and approximately 70% of symptoms presented in menopausal women, relate to vasomotor instability. This includes hot flashes due to inappropriate stimulation of the body’s heat-releasing mechanisms by the hypothalamus, and can last up to 2 years in women. Vasomotor instability can also cause vasodilation, redness, palpitations, and tachycardia. Vasomotor instability can be severe at night, during stress, or when eating hot or spicy foods.
Urogenital Changes
Urogenital changes are marked by vaginal dryness, vaginal irritation, and itching. Loss of vaginal elasticity, size, vascularization, and decrease in vaginal acidity occur, leading to dyspareunia, or painful intercourse.
The atrophy of external genitalia occurs, the labia majora lose its fat, and the labia minora lose pigmentation and became pale. Weakness of the pelvic ligaments increases the tendency of uterine prolapse. Atrophy of the urethra and bladder mucosa occurs, leading to loss of urinary wall elasticity and urinary incontinence. Urogenital atrophy can cause recurrent genital and urinary tract infections.
Cardiovascular Changes
Estrogen deficiency also increases the incidences of cardiovascular disease. In non-menopausal women, estrogen can stimulate coronary and cerebral blood flow and affect the lipid profile by increasing the HDL/LDL ratio and inhibiting plaque formation. As estrogen decreases in menopause, the HDL/LDL ratio decreases, and LDL levels rise, increasing the potential for heart attacks and strokes.
Skin Changes
Other physical symptoms of postmenopausal women include an increase in facial hair due to a relative increase in androgens, atrophy of glandular tissue in the mammary glands and its replacement by fatty tissue, and the loss of collagen fibers in the dermis, leading to thin, dry skin with dark spots. Low estrogen at menopause could also decrease cognitive function and lead to mood instability.
Osteoporosis
There is a direct relationship between the lack of estrogen and osteoporosis. An individual experiencing menopause has a high chance to develop osteoporosis due to decreased estrogen levels. Osteoporosis is usually accelerated 5 to 7 years after menopause. An activation of osteoclast bone cells is increased, leading to a decrease in bone density and loss of bone matrix and minerals.
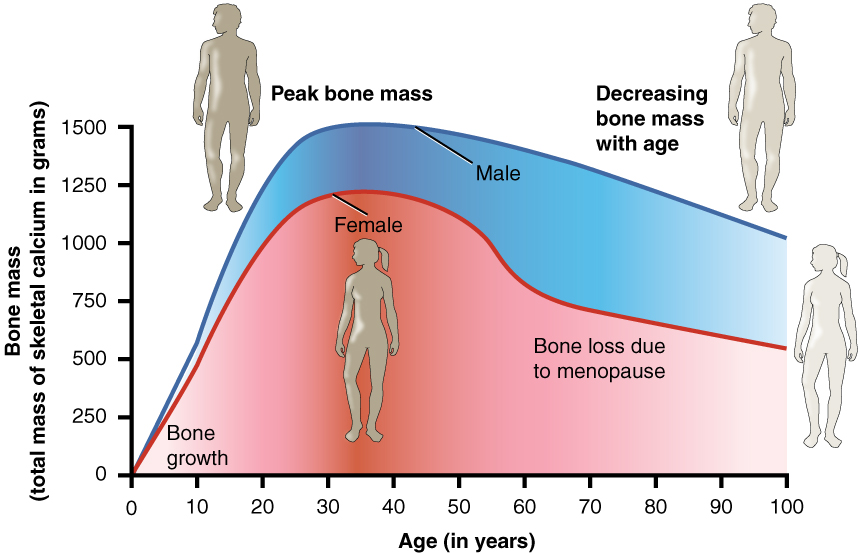
Menopausal women have a high tendency to have brittle bones and an increased risk of pathologic bone fractures and spinal deformities. Kyphosis may be developed. Osteoporosis can be prevented by increasing calcium and protein intake along with exercise. Estrogen hormones may be recommended in severe cases.
Estrogen Replacement Therapy (ERT)
To reverse the effects of menopause, some women may be advised to partake in estrogen replacement therapy (ERT). ERT significantly improves vasomotor instability, night sweats, and hot flashes. It also relieves most urogenital symptoms, dryness, itching, and pain during sex. However, ERT does not relieve vaginal stenosis. ERT can also relieve depression, insomnia, and improve mood changes. Estrogen replacement plays a vital role in inhibiting osteoclast activity, preventing bone resorption and bone loss. Thus, estrogen replacement helps in reducing the incidence of wrist, hip, and vertebral fractures.
Estrogen replacement also increases the survival rate in menopausal women with a previous coronary stenosis or heart attack. It lowers blood cholesterol and increases coronary blood flow, causing a 50% reduction in cardiovascular danger and reducing the risk of stroke.
Estrogen Replacement and Cancer Development
Correlating estrogen intake and cancer development is controversial. While estrogen replacement can reduce the risk of colon cancer, an over-intake of estrogen stimulates endometrial cell proliferation, leading to endometrial hypoplasia and endometrial cancer. Studies have also shown that the prolonged intake of estrogen more than 10 years could increase the risk for breast cancer development.
Andropause
Menopause in men starts with the decrease in androgen, called andropause. Andropause does not occur as an abrupt and noticeable event like in women, but it occurs gradually. Androgen (Testosterone) levels begin to decline gradually around the age of 40, about 1% per year. That decline is not enough to account for any decrease in libido or erectile function. However, as testosterone level continues to decline with advanced age, facial hair growth may decrease, the penis and scrotum may shrink, a slight decrease in libido may occur, and erections may take a longer time to achieve.
Male aging may also be accompanied by some changes in adrenal function. Adrenal glands androgenic hormones may continue decreasing, leading to decreased vigor and muscular flexibility, and a decline in muscle mass and strength. The chance of osteoporosis in men also increases.
Research has suggested that the administration of the steroid DHEAS in middle-aged men can increase lean body mass. However, that may lead to a potential enlargement of the prostate, increase of testicular shrinkage, and limited sperm production. Its administration should be taken under extreme supervision.
Image Sources
- Figure 1. “Hormones during the menstrual cycle” was developed for this volume and available under the same license.
- Figure 2. “Graph showing relationship between age and bone mass” is taken from OpenStax Anatomy & Physiology, licensed CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/.

