Female Endocrinology
Hormones of the Menstrual Cycle
The hormonal control of reproduction in females is complex, requiring the maturation of the hypothalamo-hyphophyseal axis, the connection between the hypothalamus and pituitary gland.
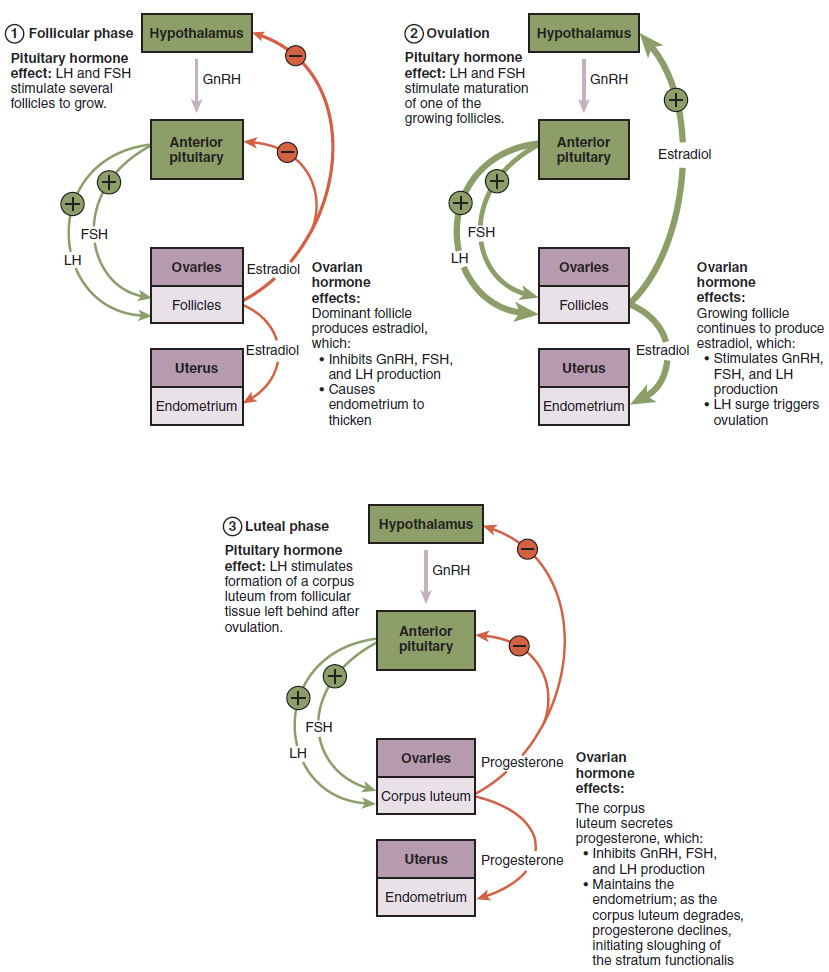
The hypothalamus stimulates the pulsatile release of GnRH, which stimulates LH and FSH release from anterior pituitary. FSH stimulates the development of egg cells, called ova, which develop in structures called follicles. Follicle cells produce estrogen and inhibin, which inhibits FSH production. LH also plays a role in the development of ova, the induction of ovulation, andthe stimulation of estradiol and progesterone production by the ovaries. Progesterone inhibits LH production. The maturation of the hypothalamo-hyphophyseal axis typically occurs 2 years after puberty, and is associated with regular menstruation cycles.
Estrogens and progesterone are sex hormones (steroid hormones) derived from cholesterol and released from the developing ovarian follicles. Estrogen is the reproductive hormone in females that assists in endometrial regrowth, ovulation, and calcium absorption; it is also responsible for the secondary sexual characteristics of females. These include breast development, flaring of the hips, and a shorter period necessary for bone maturation. Progesterone assists in endometrial growth and complete endometrial layer maturation, and inhibition of FSH and LH release. Both estrogen and progesterone prepare the body for pregnancy and regulate the menstrual cycle.
Menstrual Cycle
The cycle consists of two parts, the ovarian and uterine cycles. The ovarian cycle governs the preparation of endocrine gonads and the release of eggs, while the uterine cycle governs the preparation and maintenance of the uterine lining. These two cycles occur concurrently and are coordinated over a 22–32-day cycle, with an average length of 28 days (Figure 1).
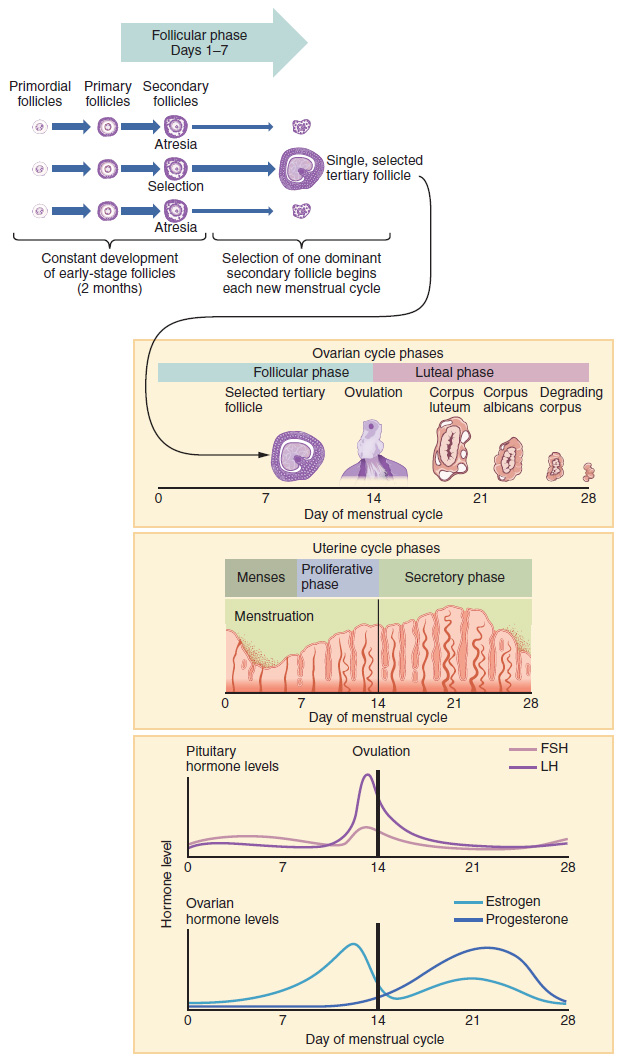
Ovarian Cycle; Pituitary-Ovarian Hormonal Effect
Follicular phase
The follicular phase is the first phase of the ovarian cycle, preparing the egg for ovulation. The phase manifests by slowly rising levels of FSH and LH from the anterior pituitary. The release of FSH and LH causes the growth of follicles on the surface of the ovary. FSH is vital for the development and maturation of the follicles. FSH is required to synthetize theca cells at the periphery of the follicle to LH. LH then acts on the surrounding theca cells, stimulating androgen synthesis. FSH also acts on follicular granulosa cells and stimulates their uptake of androgen and the conversion of androgen into estrogen.
The continued rising of ovarian estrogen levels further increases FSH production and the growth of the follicles. Once estrogen reaches a peak and its threshold causes a negative effect at the pituitary and hypothalamus, the level of FSH drops and no more follicle maturation occurs. At the same time, the level of inhibin released from follicular cells increases, which inhibits the release of FSH from the anterior pituitary. The drop of FSH stops further maturation of the follicles.
Ovulation
The surge of estrogen secretion at this time is responsible for the mid-cycle surge of LH. A concentration of 200 pg/ml or more of estrogen is necessary to produce a positive feedback effect on LH release, and it should be sustained for about 50 hours. Ovulation occurs about 29 to 39 hours after the peak of LH. At this time, the mature follicle ruptures and releases its egg with its surrounding layers. The follicles that did not rupture degenerate, and their eggs are lost. The level of estrogen decreases when the extra follicles degenerate.
Luteal phase
After ovulation, LH stimulates corpus luteum follicle formation, and the follicular cells produce estrogen and progesterone. The increased level of progesterone drops LH at the pituitary and hypothalamic levels and prevents further ovulation, a negative feedback effect. At the same time, the release of estrogen and progesterone out of the ovary influences the development of the endometrial lining of the uterus to support pregnancy. If fertilization and pregnancy do not occur, 14 days after ovulation, the corpus luteum degenerates. A fibrous tissue corpus albicans follicle develops and progesterone levels drop. With the decreased level of progesterone, the lining of the superficial endometrial layer is sloughed off. This is the inception of menstrual bleeding, and the menstrual phase of the uterine cycle.
The Uterine Cycle
The uterine cycle consists of the menstrual, proliferative, and secretory phases. Figure 2 visually compares the ovarian and uterine cycles and Figure 1 shows the commensurate hormone levels in each.
Menstrual phase
High progesterone during the luteal phase stimulates the release of prostaglandin from endometrium cells. Prostaglandins are a powerful vasoconstrictor of the smooth muscle of blood vessels. If there is no fertilization, prostaglandin causes the intermittent contraction of helical (spiral) arteries and decreases blood supply to the functionalis endometrial layer. The endometrial cells became anoxic, bacteria invades the dead endometrial layer, and the superficial layer dies (necrosis).
A sudden dilatation of the helical vessels follows as the vessels rupture. Hemorrhagic discharge, which includes blood associated with sloughed off dead functionalis layer and bacteria, is released through the vagina during menstruation, also referred to as menses. The first menses after puberty is called menarche. During this process, the basal endometrial cells remain intact.
This bleeding phase takes approximately 3-5 days. After that time, estrogen levels rise and the menstrual cycle enters the proliferative phase.
Proliferative phase
The proliferative phase starts with the end of the menstrual flow from day 4 to day 14 of the menstrual cycle. The released FSH and estrogen influence the reconstruction of the functionalis layer. The endometrium begins to regrow, replacing the blood vessels and glands that deteriorated during the end of the last cycle. Endometrial epithelial cells proliferate and reach about 2-3mm in length. Endometrial glands grow and straighten. Cells are active and start glycogen accumulation. Spiral arteries lengthen but do not reach the upper third of the endometrial layer. By day 14, the functionalis layer becomes fully restored and ovulation occurs. The ovarian cycle enters its luteal phase, and the uterine cycle enters its secretory phase.
Secretory phase (Luteal phase)
The luteal phase starts on day 15-25 of the menstrual cycle. The secretory and luteal phases are under the influence of LH and progesterone. After ovulation, the cells in the follicle undergo physical changes and produce the corpus luteum. The corpus luteum produces estrogen and progesterone. Progesterone facilitates the complete construction and differentiation of the endometrial layer. Glands are hypertrophy, cells become convoluted, and glycogen and mucoid production increase within the glands. Spiral arteries elongate and extend into superficial layers. The endometrial lining reaches its full thickness of around 5mm. At this stage, the uterus is prepared to accept a fertilized egg (implantation).
Indeed, if an embryo implants, signals are sent to the corpus luteum to continue secreting progesterone to maintain the endometrium and the pregnancy. If an embryo does not implant, no signal is sent to the corpus luteum and it degrades, ceasing progesterone production and ending the luteal phase. Without progesterone, the endometrium thins and, under the influence of prostaglandins, the spiral arteries of the endometrium constrict and rupture as menstruation occurs (initiating the next menstrual cycle). The decrease in progesterone also allows the hypothalamus to send GnRH to the anterior pituitary, releasing FSH and LH and starting the cycles again.
Clinical Correlation
Contraception and Inhibition of Ovulation
Long-term use of high concentrations of estrogen and progesterone, as with oral contraceptive pills, can lead to pituitary suppression. High estrogen levels cause a negative feedback effect on FSH, halting maturation of the follicle, while high progesterone levels causes a negative feedback effect on LH, and inhibits ovulation.
Estrogen and Endometrial hyperplasia
As estrogen is responsible for endometrial layer growth and proliferation, the building hormone, it is considered a highly mitotic hormone. Conditions with high endogenous or exogenous levels of estrogen may lead to endometrial cell hyperplasia and cancer development.
Take Home Message
- The menstrual cycle consists of ovarian and uterine cycles.
- Ovarian granulosa cells and theca cells work together to produce estrogen under the influence of FSH and LH.
- Theca cells are the source of ovarian androgens.
- High progesterone stimulates endometrial cells to secret prostaglandin, a powerful vasoconstrictor.
- Estrogen is the building hormone that reconstructs the endometrial cells; progesterone is responsible for differentiation and full maturation of the endometrium.

