The Male Reproductive System
Accessory Glands
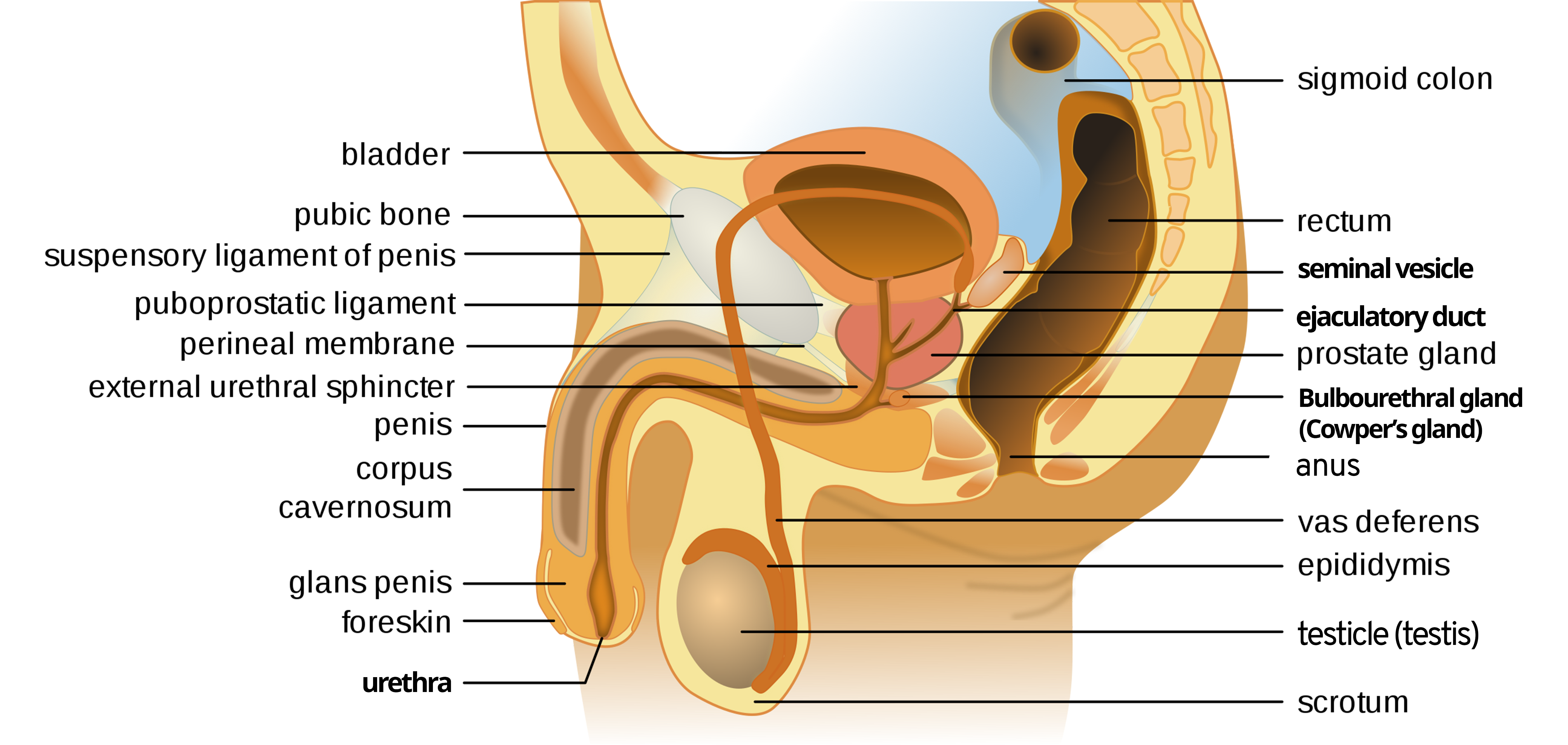
There are three glands that secrete fluids and mix with sperms to create seminal fluid. The secretions nourish the sperm and neutralize the acidity of the vagina. These three glands are the seminal vesicles, the prostate, and the bulbourethral glands.
Seminal Vesicles
Paired seminal vesicles are located on the posterior surface of the urinary bladder, lateral to the ampulla of the ductus deferens. As sperm pass through the ampulla of the ductus deferens at ejaculation, they mix with fluid from the associated seminal vesicle (Figure 1).
The paired seminal vesicles are glands that contribute approximately 75% of semen by volume. Seminal vesicles secrete whitish yellow, thick and viscous fluid. The fluid contains large amounts of fructose for the sperms’ nourishment and prostaglandins, which are used by the sperms’ mitochondria to generate ATP to allow movement through the female reproductive tract. The secretion of seminal vesicles is under the influence of testosterone.
The seminal fluid contains both sperm and seminal vesicle secretions. This fluid moves into the associated ejaculatory duct, a short structure formed from the ampulla of the ductus deferens and the duct of the seminal vesicle. The paired ejaculatory ducts transport the seminal fluid into prostatic urethra which runs through the prostate gland.
Prostate Gland
The prostate gland is a centrally located gland that sits anterior to the rectum, inferior to the bladder, and surrounding the prostatic urethra (the portion of the urethra that runs within the prostate). The gland is the size of a walnut and is formed of both muscular and glandular tissues. The glandular tissue runs in three concentric layers of 30–50 tubuloalveolar glandular tissues. The mucosal glands open directly into the urethra. The submucosal layer is larger than the mucosal and has short ducts that open into the urethra. The main mucosal glands have long ducts that open into the prostatic urethra. Prostatic secretion contributes to 20–30% of seminal fluid and is under the influence of testosterone. The prostate normally doubles in size during puberty. At approximately age 25, it gradually begins to enlarge again. This enlargement does not usually cause problems.
The prostatic secretion contains mucin and citric acid, providing nutrients for sperms. It is slightly acidic to partially neutralize the alkaline nature of seminal vesicle fluid. Prostatic secretion is rich in prostatic-specific antigen (PSA), an enzyme that helps liquify the viscosity of seminal fluid and achieve good sperm mobility. The final secreted fluid in the prostatic urethra is now called semen, which helps sperms pass farther into the female reproductive tract.
Clinical Correlation
Benign prostatic hyperplasia (BPH)
Abnormal growth of the prostate or benign prostatic hypertrophy (BPH) is usually caused by the enlargement of the mucosal and submucosal parts of the glands that lead to constriction of the urethra as it passes through the middle of the prostate gland. Prostatic hypertrophy can cause a number of lower urinary tract symptoms, such as a frequent and intense urge to urinate, a weak stream, and a sensation that the bladder has not emptied completely. By age 60, approximately 40 percent of men have some degree of BPH. By age 80, the number of affected individuals has jumped to as many as 80 percent. Treatments for BPH attempt to relieve the pressure on the urethra so that urine can flow more normally. Mild to moderate symptoms are treated with medication, whereas severe enlargement of the prostate is treated by surgery in which a portion of the prostate tissue is removed.
Prostatic Adenocarcinoma
Prostate cancer is the second most common cancer in men. Prostatic carcinoma usually arises from the largest and outer part of the glands, the prostatic bulk, that open via long ducts to the urethra. Some forms of prostate cancer grow very slowly and thus may not ever require treatment. In contrast, aggressive forms of prostate cancer can cause metastasis to vulnerable organs like the lungs and brain. There is no link between BPH and prostate cancer, but the symptoms are similar. Prostate cancer is detected by a medical history, a blood test, and a rectal exam that allows physicians to palpate the prostate and check for unusual nodular masses. If a mass is detected, the cancer diagnosis is confirmed by a biopsy of the cells.
Bulbourethral Glands
The final addition to semen less than 5% is made by two bulbourethral glands (or Cowper’s glands), Located in the urogenital diaphragm on either side of the membranous urethra. The glands release a thick, salty fluid that lubricates the end of the spongy urethra and the vagina and helps to clean urine residues from the penile urethra. The fluid from these accessory glands is released after the male becomes sexually aroused and shortly before the release of the semen. It is sometimes called pre-ejaculate for this reason. It is important to note that, in addition to the lubricating proteins, bulbourethral fluid can pick up sperm already present in the urethra, and therefore it may be able to cause pregnancy.
Take Home Message
- Accessory glands function under the influence of testosterone and help in the production of seminal fluids.
- Prostatic secretion neutralizes the alkaline nature of the seminal fluid.
Image Sources
- Figure 1. “Male anatomy svg, labeled” is from Tsaitgaist via Wikimedia Commons, licensed CC BY 3.0.

