Pelvic Pain
Pelvic Pain
Pelvic pain can have many causes, including the digestive, urinary, or reproductive system. It may be attributed to factors such as ovulation, dysmenorrhea, or sexually transmitted diseases (STDs), among others. Given the diverse range of underlying causes, various treatment options are available to address these symptoms. We will explore several reproductive factors and conditions linked to pelvic pain and discomfort in this chapter.
Pelvic pain unrelated to pregnancy
Menstrual-related pain
Pelvic pain that is unrelated to pregnancy may be caused by ovulation or dysmenorrhea. Pain around the time of ovulation can occur for a few hours and may last 2 days.
Dysmenorrhea is severe pain caused by menstrual cramps. It is theorized that excess prostaglandin causes smooth muscle contractions, leading to dysmenorrhea. These painful menses are typically observed in the first five years of ovulatory menstrual cycles, and improve with age. Dysmenorrhea affects over 50% of all post-pubescent women. To manage the pain, prostaglandin inhibition or the suppression of cycles is sought. Other methods for managing the pain include the use of heat, mild analgesics, and exercise.
Pelvic Inflammatory Disease PID
Pelvic inflammatory disease (PID) is an infection affecting the female reproductive system, typically resulting from pelvic infections transmitted through sexual contact, such as gonorrhea or chlamydia. The use of an intrauterine device (IUD) for contraception can also elevate the risk of PID. On the other hand, oral contraception may offer some protection, as it disrupts cervical secretions and hinders the attachment of these organisms to endometrial cells. PID, if left untreated, can lead to severe complications, including chronic pain, infertility, ectopic pregnancies, and, in extreme cases, even death.
Endometriosis
Endometriosis is when tissue that normally lines the endometrium grows outside of the uterus, causing pelvic pain (See Figure 1). This can occur at any time throughout female reproductive years.
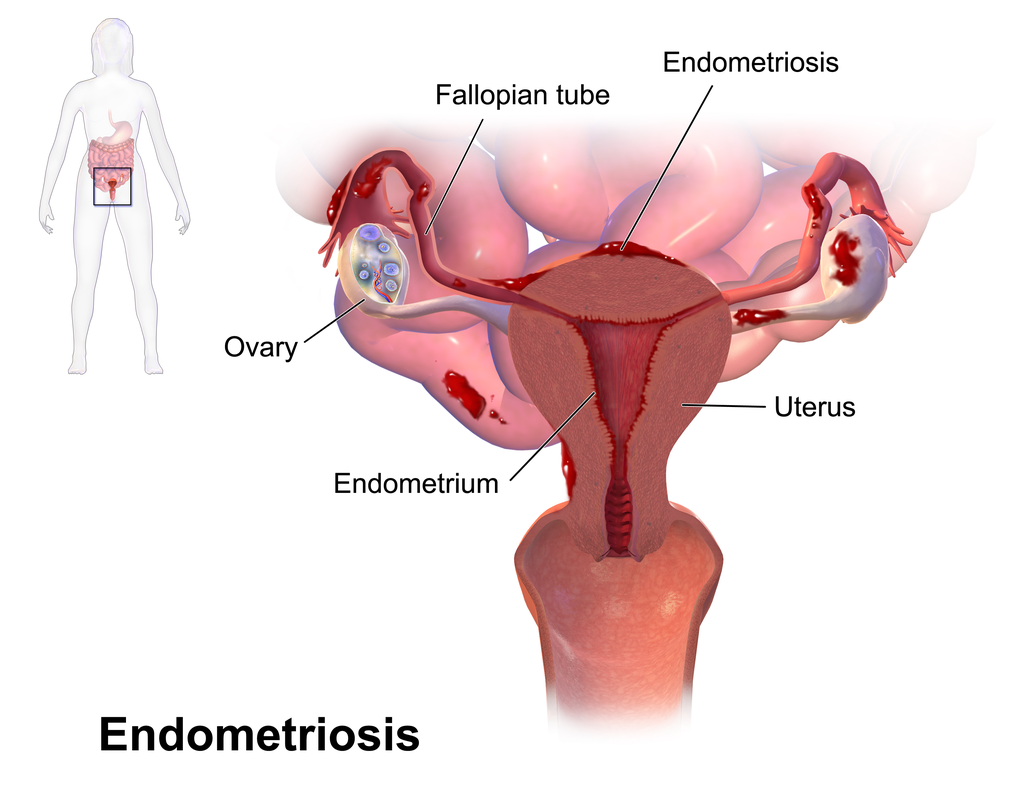
Endometriosis can cause cyclic pain, dysmenorrhea, and severe dyspareunia, or painful intercourse. If a female has endometriosis, she has a 30-40% chance of being infertile. Endometriosis can cause a female to become infertile by trapping the ovum, or the cytokine and prostaglandin production that may interrupt the ovulation, tubal function, and luteal phase detection. Management of endometriosis typically involves treatment through hormonal therapies or excision surgery.
Reproductive Tumor
Reproductive tumors, such as ovarian (or testicular in males), uterine, or cervical tumors, can lead to pelvic pain. Several treatment options are available for reproductive tumors, including surgery, chemotherapy, radiation therapy, and targeted therapy. The choice of treatment depends on many factors, like the type and stage of the tumor, the patient’s overall health, and individual preferences. It is paramount to stress the significance of early detection via regular screenings, immunization, and vaccination. Additionally, a proactive approach to understanding one’s genetic predisposition and making lifestyle choices conducive to overall well-being can considerably reduce the risk of reproductive tumors and enhance long-term health.
Pelvic pain related to pregnancy
Pelvic pain in females related to pregnancy can be attributed to conditions such as abortions or ectopic pregnancies.
Abortions (Miscarriage)
Miscarriage, also referred to as pregnancy loss, is the spontaneous termination of a pregnancy before reaching the 20th week of gestation. It affects approximately 10-20% of known pregnancies and can occur due to various factors, including chromosomal irregularities, hormonal imbalances, and specific health conditions.
Symptoms of a miscarriage often include pelvic discomfort, which may range from mild to severe and is frequently accompanied by bleeding. Bleeding is a prevalent indicator of a miscarriage, varying in intensity from light spotting to heavy discharge. In some instances, the body naturally expels the pregnancy tissue without the need for medical intervention, a practice known as expectant management, commonly employed for early miscarriages.
In situations where the miscarriage is incomplete or presents complications, a healthcare provider may recommend medication to facilitate the expulsion of the remaining tissue. Alternatively, a surgical procedure, such as dilation and curettage (D&C) or aspiration, may be necessary to remove the pregnancy tissue.
To help individuals and couples navigate the emotional impact of pregnancy loss, grief counseling and participation in support groups can provide valuable assistance.
Ectopic Pregnancy
An ectopic pregnancy occurs when the implantation of a zygote takes place outside of the uterus or in an abnormal location within the uterus (See Figure 2). In 95% of ectopic pregnancies occur in the fallopian tubes, but they can also occur in the abdomen or cervix. The pain may be characterized as unilateral or generalized, crampy or sharp. Vaginal bleeding and spotting can also occur. Certain individuals may also encounter nonspecific symptoms, such as an unusual urge to defecate, which can occasionally overlap with common pregnancy signs.
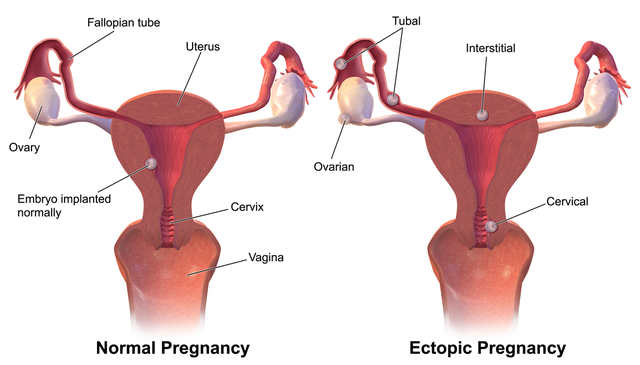
The risk of an ectopic pregnancy is elevated in cases of a previous ectopic pregnancy, a history of pelvic infection (e.g., chlamydia and gonorrhea), the use of an intrauterine device (IUD), the presence of endometriosis, or factors that impede ovum transport, including the use of oral contraceptive pills (OCP) or smoking.
Image Sources
- Figure 1. “Endometriosis” is from Bruce Blaus via Wikimedia Commons, licensed CC BY 3.0.
- Figure 2. “Ectopic Pregnancy” is from Bruce Blaus via Wikimedia Commons, licensed CC BY SA 4.0.

