Normal Pregnancy
Endocrinology of Pregnancy
Pregnancy is the period during which a fetus develops inside the womb. Pregnancy usually lasts about 40 weeks, or just over 9 months, as measured from the last menstrual period to delivery. These 40 weeks are broken up into trimesters. The first trimester starts on the first day of the pregnant person’s last period and ends on the last day of week 12. The second trimester starts on week 13 and ends on the last day of week 27. Finally, the third trimester starts on the first day of week 28 and ends sometime during the 38th to 40th week of pregnancy.
Hormonal Changes During Pregnancy
Hormones play a major role throughout pregnancy. Different hormonal levels and types are found in pregnant women compared to non-pregnant women. Some of these hormones are newly found in the pregnant individual, or their levels may be varied compared to non-pregnant people. The sources of these hormones may come from the newly developed placenta, the fetus, or from the mother’s tissues.
The hormones that have been detected during pregnancy have been studied to distinguish between normal and abnormal pregnancies, detect fetal conditions, and identify any complications that may occur during pregnancy. Significant hormones present during pregnancy are listed below.
Human Chorionic Gonadotropin (HCG)
This hormone is produced by the syncytiotrophoblast of the placenta. HCG can be detected as early as six to eight days following conception and throughout the rest of the pregnancy. It can be detected in blood first, and is later noticeable in urine. HCG has a specific pattern during pregnancy. Its levels rise rapidly 8 days after conception, doubling every two to three days and reaching its peak at 80 days after fertilization. Then it drops to a plateau for the remainder of the pregnancy.
HCG is used to detect both normal uterine and ectopic pregnancies. Its pattern and peak run at a much lower level in ectopic pregnancies than in normal pregnancies, and in conditions with poor placental function or fetal demise. HCG levels will be duplicated in multiple pregnancies with multiple placenta, and can reach very high levels in trophoblastic neoplasms. During pregnancy, HCG functions to prompt the corpus luteum to produce progesterone, and prompts male fetus’ Leydig cells to produce testosterone. HCG is similar to LH hormones and also helps induce ovulation.
Human placental Lactogen (hPL)
Like HCG, this hormone is also produced by the syncytiotrophoblast of the placenta. hPL is formed as early as three weeks post conception and can be detected in a maternal bloodstream around six weeks post conception. hPL rises steadily in the first and second trimesters, and it disappears rapidly after delivery. hPL is a growth hormone, and its level correlates directly to the weight of the fetus and placenta. Very high maternal levels of hPL are often associated with multiple gestation, twins, or triplets.
The hPL has a significant effect on fetal development. It favors protein synthesis and ensures a source of amino acids for fetal growth. It promotes the formation of insulin-like growth factors and induces the growth of all fetal tissues.
In the mother, hPl has a diabetogenic effect. It induces insulin resistance and carbohydrate intolerance, inhibiting glucose uptake in the mother. This can lead to the elevation of maternal blood sugar in those predisposed to high blood sugar.
Prolactin
Prolactin is a hormone produced by both the mother’s and fetus’s pituitary glands. It is also produced by the decidualized tissues of the maternal endometrium. Prolactin can be detected in maternal serum as well as maternal amniotic fluid. Maternal prolactin levels rise to a maximum of 100ng/ml near term.
Prolactin stimulates the production of milk by the mammary glands and prepares them for lactation after birth. The decidual prolactin secreted by the endometrium is thought to be important for electrolyte regulation of the amniotic fluids.
Higher levels of prolactin in a non-pregnant woman would indicate a hyperactive or tumor function of the pituitary gland.
Alpha-fetoprotein (AFP)
AFP is a hormone produced by the yolk sac and liver of the fetus. It can be detected in the amniotic fluid at five to twelve weeks following conception and in the pregnant woman’s bloodstream around 15 to 17 weeks following conception. The exact role of alpha-fetoprotein remains a question, but it is known that it is mainly found in large amounts in the fetus’s central nervous system (CNS). Abnormal direct contact of fetal CNS with the amniotic fluid, as in neural tubal defect, results in elevated amniotic fluid and maternal blood levels of alpha-fetoprotein. In pregnancies involving a fetus with Down’s syndrome (DS), the level of alpha-fetoprotein measured in maternal serum and amniotic fluid is reduced to about 70 percent of the level attained in typical pregnancies.
Progesterone
Progesterone is produced by the corpus luteum follicle. In a non-conception cycle, progesterone is produced during ovulation at an amount of up to 25 mg per day. In the conception cycle, during the luteal phase, hCG stimulates more progesterone secretion by the corpus luteum and progesterone levels increase gradually and slowly. Progesterone continues to be produced by the corpus luteum until 7 to 10 weeks of gestation. Around 10 weeks post-conception, the placenta takes form and supplements the corpus luteum. Progesterone continues to be produced by the placenta until the delivery time. Its level is increased rapidly during pregnancy until the time of parturition up to -250mg/day. A very high level of progesterone could be indicative of multiple gestation.
Progesterone is required for decidualization and preparation of the endometrium for implantation. It also helps to maintain a relaxed myometrium until labor occurs. Interruption of progesterone levels or its action may lead to the termination of pregnancy. Progesterone serves as a major precursor to critical fetal hormones during pregnancy. The fetal adrenal cortex glands uses placental progesterone as a precursor for corticosteroids, and fetus testes use placental progesterone as a precursor for testosterone.
Estrogen
The estrogen hormone is unique in that the mother, placenta, and fetus produce it. Estriol, the primary form of estrogen involved in pregnancy, is synthesized in the second trimester and is produced in increasing amounts until term. This surge in estriol is what causes the total amount of estrogen to increase 1,000 times more than that of a non-pregnant woman. Estrogen levels are indicative of both a fetus’s and placenta’s well-being. If the level of estrogen appears low or does not increase from the second trimester until term as expected, this may indicate pregnancy complications, fetal demise, or fetal growth retardation.
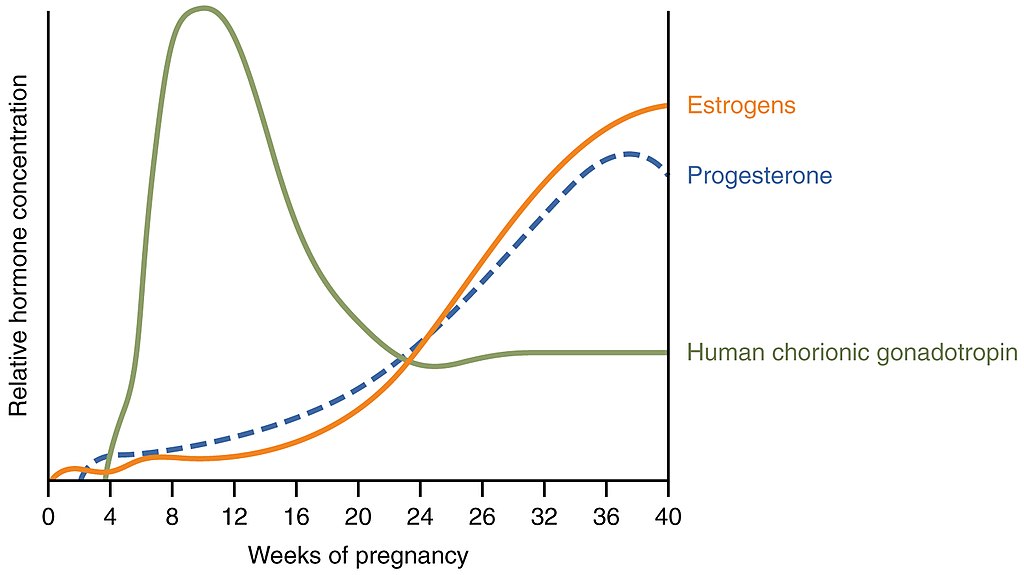
Image Sources
- Figure 1. “Hormones during pregnancy” is from OpenStax Anatomy & Physiology, licensed CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction

