Infertility
Female Infertility Evaluation
Ovarian Factor
There are several methods to detect the presence of ovulatory cycles. By employing these methods, healthcare professionals can assess and detect potential ovarian factors contributing to infertility.
- Monitoring Menstrual Cycles: Regular menstrual cycles, accompanied by premenstrual symptoms, often serve as a reliable indicator of ovulation.
- Basal Body Temperature (BBT) Tracking: A BBT increase of at least 0.4°F over the temperature recorded during the proliferative phase is generally considered within the normal range, suggesting the occurrence of ovulation.
- Serum Progesterone Analysis: Obtaining a single serum progesterone value above 4 ng/ml between days 19 and 23 of the menstrual cycle can be indicative of ovulation.
- Urinary LH Surge Assessment: The measurement of urinary luteinizing hormone (LH) surge, accomplished through various commercially available ELISA home test kits, can prospectively predict both the presence and timing of ovulation. These tests help identify the surge in LH, a hormone that triggers ovulation.
On the other hand, monitoring the common causes of anovulation can also be detected through physical examination and clinical assessment.
Frequent Causes of Anovulation
- Fluctuations in Body Weight: Anovulation can occur due to significant deviations in body weight, both in cases of excessive weight gain and extreme weight loss.
- Polycystic Ovary Syndrome (PCOS): Chronic hyperandrogenic anovulation, often associated with PCOS, is a common cause of disrupted ovulation patterns.
- Emotional Stress: High levels of emotional stress can disrupt the regularity of menstrual cycles, leading to anovulation.
- Medications: Certain medications, especially those affecting hormone levels, can contribute to anovulation.
- Systemic Illness: Chronic or severe systemic illnesses can disrupt the body’s hormonal balance, potentially leading to anovulation.
- Structural Lesions Affecting the Hypothalamic-Pituitary-Ovarian Axis: Structural abnormalities in the hypothalamic-pituitary-ovarian axis can hinder the normal ovulatory process.
- Initial Blood Tests: Initial blood evaluations should typically include measuring thyroid-stimulating hormone (TSH) and prolactin levels routinely. Additionally, assessing follicle-stimulating hormone (FSH) levels and total testosterone can provide valuable insights into the underlying issues.
- Serial Ultrasound Examinations: Serial ultrasound examinations are often conducted to monitor and ascertain the collapse of ovarian follicles. This helps in tracking the development and release of eggs during the menstrual cycle, aiding in the diagnosis and management of anovulation-related issues.
Tubal Factor
It’s important to consider that approximately 20-30% of cases can be attributed to pelvic abnormalities, such as tubal occlusion, adhesions, and severe endometriosis.
One diagnostic approach to rule out tubal factor infertility is the use of a Hysterosalpingogram (HSG). This diagnostic test should ideally be conducted relatively early in the infertility investigation, following a semen analysis.
The primary purposes of an HSG are:
- Evaluation of Tubal Patency: Using transuterine water-soluble contrast instillation under fluoroscopic visualization helps assess whether the fallopian tubes are open and unobstructed.
- Assessment of Uterine Cavity: Additionally, the HSG can provide valuable information about the contour and adequacy of the uterine cavity.
Hysterosalpingogram (HSG) is typically performed in the follicular phase of the menstrual cycle before ovulation. In cases where the HSG results are inconclusive or further investigation is warranted, laparoscopy may be recommended.
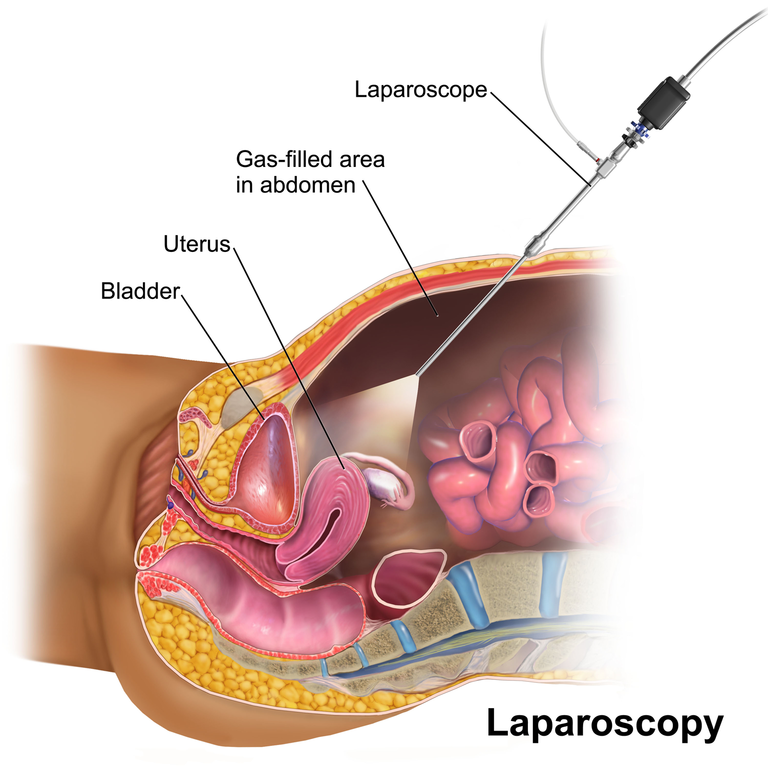
Laparoscopy
Laparoscopy is a surgical procedure that allows for a direct visual examination of the pelvic organs. It can provide a more detailed assessment of pelvic abnormalities, including the condition of the fallopian tubes, adhesions, and endometriosis. Diagnostic laparoscopy involves the insertion of a fiberoptic scope through small incisions into the abdominal cavity, and is typically performed under general anesthesia.
During a diagnostic laparoscopy procedure, here’s what you can generally expect:
- Exploration of the Pelvis: Laparoscopy allows the surgeon to explore and visually examine the pelvic region. This can provide insights into potential causes of infertility, such as pelvic adhesions, endometriosis, or structural abnormalities.
- Hysteroscope for Uterine Cavity Examination: In some cases, a hysteroscope (a thin, lighted tube with a camera) can also be utilized during laparoscopy to examine the uterine cavity. This helps in assessing the condition of the uterine lining and identifying any abnormalities.
- Transvaginal Contrast Injection: To assess the patency of the fallopian tubes, a contrast dye can be injected through the cervix transvaginally via a canula. This allows for the visualization of dye passing through the fimbriated ends of patent (open) fallopian tubes when observed laparoscopically.
Endometrial Factor
An endometrial biopsy can be used to assess endometrial factors. In the context of evaluating female infertility, it is crucial to consider the quality of the endometrium, which must be suitable to facilitate implantation. If it is not, this condition is referred to as luteal phase inadequacy (LPI). The assessment of endometrial factors involves:
- Histological Pattern of the Endometrium: This assessment is based on the development of endometrial glands and stroma. An office biopsy procedure is typically performed using an endometrial sample collected from the upper part of the uterus just before the onset of menstrual bleeding.
- Discrepancy in Timing: To diagnose luteal phase inadequacy, a significant discrepancy of 2 or more days from the norm for the day the biopsy was taken. Consistency must be observed in two consecutive menstrual cycles. The diagnosis of luteal phase inadequacy is established when there is a consistent discrepancy in endometrial development over two consecutive cycles.
Cervical Factor
When assessing cervical factor infertility, a sample of cervical mucus is typically collected at midcycle, which is the time of ovulation. The evaluation involves the following steps:
- Sample Collection: A small sample of cervical mucus is carefully aspirated (drawn into a pipette or tube) during the midcycle, which corresponds to the fertile window when ovulation is likely to occur.
- Slide Preparation: The collected cervical mucus is placed on a glass slide.
- Cover Slip Application: A cover slip is applied to the glass slide, covering the cervical mucus sample.
- Stretchability Measurement: The degree to which the cervical mucus stretches is assessed. This is done by gently lifting the cover slip and observing how far the mucus extends before breaking.
- Optimal Stretch Length: In the assessment, cervical mucus that stretches into columns measuring 8 centimeters or more is considered optimal for fertility. This indicates good quality cervical mucus that is conducive to sperm transport through the cervix and into the uterus.
- Microscopic Examination: In addition to the stretchability assessment, the cervical mucus can also be examined microscopically. Good-quality mucus appears acellular under the microscope, meaning it doesn’t contain many cells or debris. Furthermore, when dried on a slide, it forms a fern leaf-like pattern. This characteristic ferning pattern is indicative of high sodium chloride (salt) content in the mucus.
The assessment of cervical mucus quality plays a significant role in fertility evaluation, as it affects sperm transport and survival within the female reproductive tract. Healthy cervical mucus provides an environment that supports sperm motility and facilitates the journey of sperm to meet the egg for fertilization.
Image Sources
- Figure 1. “Laparascopy” is from BruceBlaus via Wikimedia Commons, licensed CC BY 3.0.

