The Female Reproductive System
Female Internal Genitalia
Ovaries
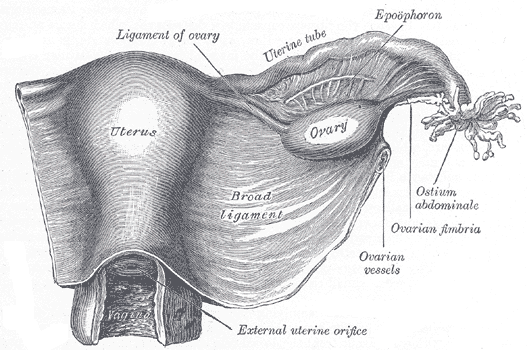
The ovaries are the female gonads (Figure 1), paired oval organs. Each is 2 to 3 cm in length and about the size of an almond. The ovaries are located within the pelvic cavity embedded in the posterior surface of the broad ligament of the uterus. They are supported by the mesovarium, an extension of the peritoneum that is continuous with the outer ovaries. The ovary itself is attached to the uterus via the ovarian ligament. Extending from the mesovarium is the suspensory ligament that connects the ovary to the lateral pelvic wall and contains the ovarian blood and lymph vessels. Loose, elongated ligaments or conditions that may lead to ligament twisting, could cut off blood supply to the ovary, pain, and necrosis of the ovarian cells (Ovarian Torsion).
The ovary comprises an outer covering of simple cuboidal epithelium called the germinal epithelium. Deep to the ovarian surface epithelium, a dense connective tissue covering called the tunica albuginea. Beneath the tunica albuginea is the cortex, the outer portion of the ovary. The ovarian cortex is composed of thousands of ovarian follicles. Each ovarian follicle consists of an oocyte surrounded by surrounded stromal cells (follicle cells or granulosa cells). Beneath the cortex lies the inner ovarian medulla, the site of blood vessels, lymph vessels, and the nerves of the ovary.
Follicular development and maturation (Folliculogenesis)
The process of follicular growth and maturation is called folliculogenesis (Figure 2), which typically leads to the ovulation of one follicle approximately every 28 days, along with death to multiple other follicles.
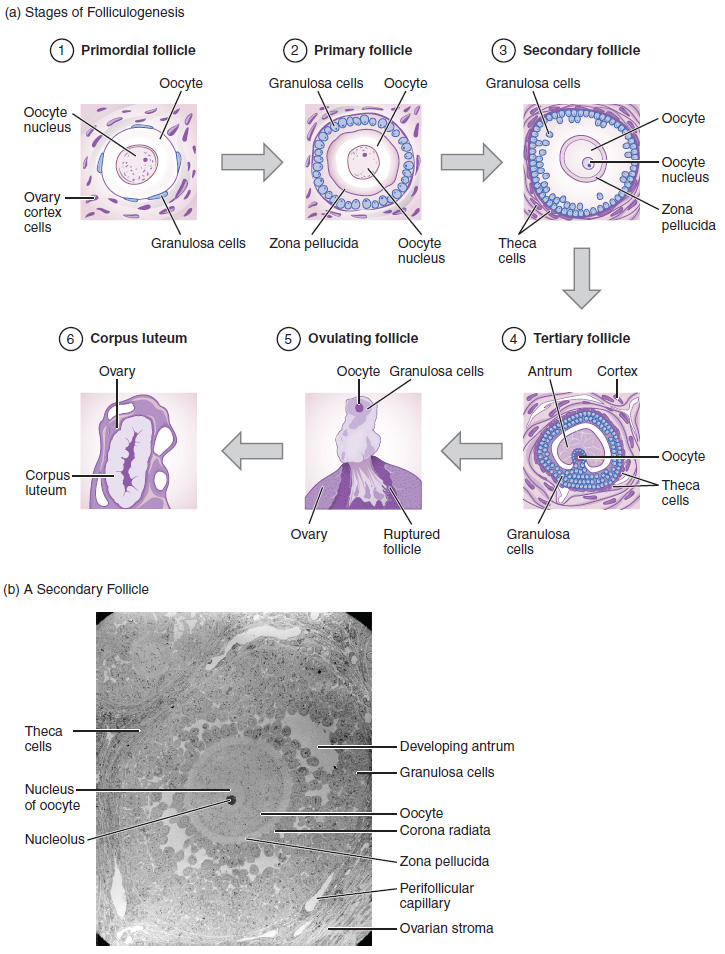
The death of ovarian follicles is called atresia and can occur at any point during follicular development. At birth, a female infant will have half a million oocytes within her ovarian follicles, and this number declines throughout life until menopause, when no follicles remain. Follicle maturation is under the effect of FSH and goes through a few stages of development. It progresses from resting primordial, to primary, to secondary and tertiary stages where ovulation occurs. The oocyte inside the follicle remains as a primary oocyte, arrested at prophase I of the first stage of meiosis until right before ovulation.
At birth, all the follicles in newborn females are small primordial follicles, a primitive type of ovarian follicle, and consists of a primary oocyte surrounded by a single layer of flattened stromal cells (Granulosa cells).
Around puberty, a few primordial follicles will respond to a recruitment signal each day through FSH hormone and join a pool of immature growing follicles. The single-layer granulosa cells become active, and transition from a flat or squamous shape to a rounded, cuboidal shape as they increase in size and proliferate, and the follicles change to primary follicles.
As FSH levels increase, the follicles continue to grow. The granulosa cells continue to divide, adding many layers of granulosa cells and the follicles increase in diameter, now called secondary follicles. The follicles still contain a primary oocyte, surrounded by many layers of follicle granulosa cells. Within the growing secondary follicle, the primary oocyte now secretes a thin acellular membrane called the zona pellucida that will play a critical role in fertilization. Two protective structures that surround the primary oocyte are developed, the zona pellucida and several layers of granulosa cells surround the oocyte, corona radiata. Several fluid-filled spaces start to develop, and the formation of the antrum begins. The fluid-filled spaces increase in volume as the follicles mature. A new outer layer of connective tissue, blood vessels, and theca cells start to develop at the periphery of the follicles — theca cells work with the granulosa cells to produce estrogens.
The thick fluid between the granulosa cells begins to collect into one large pool, and a well-developed antrum develops. A well-developed Theca cells layer is located at the periphery of the follicles. Follicles in which the antrum has become large and fully formed are considered tertiary, Mature, or Graafian follicles. Several follicles reach the tertiary stage at the same time, and most of these will undergo atresia. The one that does not die will continue to grow and develop until ovulation.
At ovulation, FSH and LH continue to increase. LH reaches its peak and stimulates the completion of meiosis I and the beginning of the second stage of meiosis of the oocyte within the follicle. Now the tertiary follicle contains the secondary oocyte, surrounded by zona pellucida and corona radiata cells layers. LH influences the rupture of the follicles and releases the secondary oocyte and its surrounding layers. Keep in mind that most follicles don’t make it to this point. In fact, roughly 99 percent of the follicles in the ovary will undergo atresia, which can occur at any stage of folliculogenesis.
If the oocyte is successfully fertilized, the resulting zygote will begin to divide into two cells, then four, and so on, as it makes its way through the uterine tube and into the uterus. There, it will implant and continue to grow. If the egg is not fertilized, it will degrade—either in the uterine tube or the uterus, where it may be shed with the next menstrual period.
After ovulation and the release of the secondary oocyte, the remaining granulosa cells multiply and form a mass of cells that are wrapped by the theca cells layer, and the follicle is now called the corpus luteum follicle. The corpus luteum follicle secretes progesterone and estrogen, which stimulates the growth of the uterine endometrium and supports the fertilized egg until the placenta is developed. 14 days after ovulation, if fertilization has not happened, degeneration of the granulosa cells will occur and the cells will be replaced by fibrous connective tissue. The follicle is then called corpus albicans.
Take home Message
- All follicles at birth are primordial follicles, with the effect of FSH hormone many follicles grow, few reach maturation and the rest die. Usually, one ruptures at the time of ovulation.
- A Tertiary mature follicle is large in diameter, containing a secondary oocyte, large antrum, and well-developed theca cell layer.
- The peak of LH hormones leads to the rupture of mature follicles at ovulation and releases the secondary oocyte and the surrounding zona pellucida and corona radiata.
Image Sources
- Figure 1. “Broad ligament” is from Gray’s Anatomy. Public domain.
- Figure 2. “Folliculogenesis” is from OpenStax Anatomy & Physiology 2E, licensed CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction (Micrograph provided by the Regents of University of Michigan Medical School © 2012)

