Birth
Diana Lang; Martha Lally; Suzanne Valentine-French; Laura Overstreet; Julie Lazzara; and Naomi H. Dan Karami
Preparation for Childbirth
Prepared childbirth refers to being in good physical condition to help provide a healthy environment for the fetus to develop, help individuals prepare to accept their new roles as parents. Additionally, parents can receive information and training that will assist them for delivery and life with the new addition to their family. Parents should learn about childbirth options and caring for a newborn before labor and delivery.[1]
One of the most common methods for preparing for childbirth is the Lamaze method. This method originated in Russia and was brought to the United States in the 1950s by Fernand Lamaze. The emphasis of this method is on teaching the woman to be in control in the process of delivery. It includes learning muscle relaxation, breathing though contractions, having a focal point (usually a picture to look at) during contractions, and having a support person who goes through the training process with the pregnant woman and serves as a coach during delivery.[2]
Choices and decisions: There are numerous decisions and choices that can be made such as what type of a practitioner will oversee one’s care, whether the delivery will occur at home or in a facility, vaginally or by Cesarean, and what, if any, pain management will be used.
Many women who give birth at hospitals use an epidural anesthesia during delivery.[3] An epidural block is a regional analgesic that can be used during labor and alleviates most pain in the lower body without slowing labor. The epidural block can be used throughout labor and has little to no effect on the baby. Medication is injected into a small space outside the spinal cord in the lower back. It takes 10 to 20 minutes for the medication to take effect. An epidural block with stronger medications, such as anesthetics, can be used shortly before a C-section or if a vaginal birth requires the use of forceps or vacuum extraction. A Cesarean section (C-section) is surgery to deliver the baby by being removed through the mother’s abdomen. Most C-sections are done when problems occur during delivery unexpectedly. These can include:
- Health problems in the mother.
- Signs of distress in the baby.
- Not enough room for the baby to go through the vagina.
- The position of the baby, such as a breech presentation where the head is not in the downward position.
C-sections are also more common among women carrying more than one fetus. This surgery is relatively safe for mother and baby, but it is considered a major surgery and carries health risks. And, it typically takes longer to recover from a C-section than from a vaginal birth. After healing, the incision may leave a weak spot in the wall of the uterus. This could cause problems with an attempted vaginal birth later. However, many women who have a C-section deliver vaginally after a C-section. Click this link to learn more about options available for the preparation of childbirth: ACOG Labor and Delivery
Stages of Birth for Vaginal Delivery
The first stage of labor is typically the longest. It begins with uterine contractions that may initially last about 30 seconds and be spaced 15-20 minutes apart. These increase in duration and frequency to more than a minute in length and about 3 to 4 minutes apart. Typically, practitioners advise that they should be called when contractions are occurring about every fine minutes. Some women experience false labor or Braxton-Hicks contractions, especially with the first child. These may come and go. They tend to diminish when the woman begins walking around. Real labor pains tend to increase with walking.
During this stage, the cervix or opening to the uterus dilates to 10 centimeters or just under four inches. This may take around 12-16 hours for first children, about 6-9 hours for women who have previously given birth, and it may take up to 24 hours for others. Labor may also begin with a discharge of blood or amniotic fluid. If the amniotic sack breaks, labor will be induced (if necessary) to reduce the risk of infection.
A baby’s arrival may need to be induced or delivered before labor begins if there is concern for the health of the mother or baby. For example:
- The mother is approaching two weeks beyond her due date and labor has not started naturally.
- The mother’s water has broken, but contractions have not begun.
- There is an infection in the mother’s uterus.
- The fetus has stopped growing at the expected pace.
- There is not enough amniotic fluid surrounding the fetus.
- The placenta peels away, either partially or completely, from the inner wall of the uterus before delivery.
- The mother has a medical condition that might put her or her baby at risk, such as high blood pressure or diabetes.[4]
The second stage involves the passage of the baby through the birth canal. This stage takes about 10-40 minutes. Contractions usually occur about every two to three minutes. The woman pushes and relaxes as directed by the medical staff. Normally the head is delivered first. The baby is then rotated so that one shoulder can come through and then the other shoulder. The rest of the baby quickly passes through. The baby’s mouth and nose are suctioned out. The umbilical cord is clamped and cut.
The third stage is generally less painful when compared to the other stages. During this stage, the placenta or afterbirth is delivered. This typically occurs within 20 minutes after the delivery of the baby. If tearing of the vagina occurred during birth, the tear may be stitched at this time.
Watch “Life’s Greatest Miracle”
Assessing the Neonate
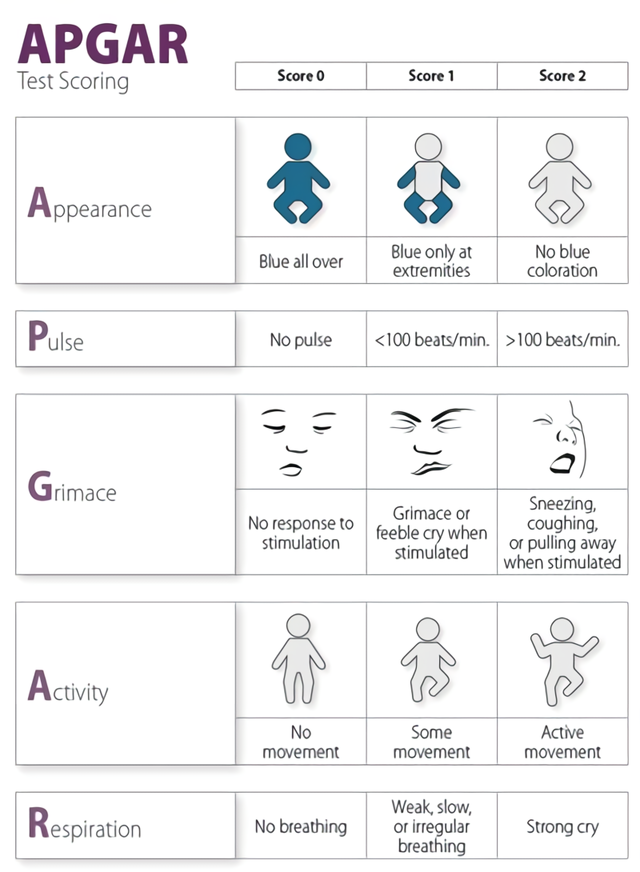
The Apgar assessment is conducted one minute and five minutes after birth by a medical professional (Figure 1). This is a very quick way to assess the newborn’s overall condition. Five measures are assessed: Heart rate, respiration, muscle tone (assessed by touching the baby’s palm), reflex response (the Babinski reflex is tested), and color. A score of 0 to 2 is given on each feature examined. An Apgar of 5 or less is cause for concern. The second Apgar should indicate improvement with a higher score.
Another way to assess the condition of the newborn is the Neonatal Behavioral Assessment Scale (NBAS). The baby’s motor development, muscle tone, and stress response are assessed. This tool has been used around the world to further assess the newborn, especially those with low Apgar scores, and to make comparisons of infants in different cultures.[5]
Problems That May Exist with a Newborn
Anoxia: Anoxia is a temporary lack of oxygen to the brain. Difficulty during delivery may lead to anoxia which can result in brain damage or in severe cases, death. Babies who suffer both low birth weight and anoxia are more likely to suffer learning disabilities later in life as well.
Low birth weight: Children are considered low birth weight if they weigh less than 5 pounds 8 ounces (2500 grams). About 8.2 percent of babies born in the United States are of low birth weight.[6] A low birth weight baby has difficulty maintaining adequate body temperature because it lacks the fat that would otherwise provide insulation. Such a baby is also at more risk for infection, and 67 percent of these babies are also preterm which can make them more at risk for respiratory infection. Very low birth weight babies (2 pounds or less) have an increased risk of developing cerebral palsy. Many causes of low birth weight are preventable with proper prenatal care.
Preterm: A newborn might also have a low birth weight if it is born at less than 37 weeks gestation, which qualifies it as a preterm baby.[7] Early birth can be triggered by anything that disrupts the mother’s system. For instance, vaginal infections can lead to premature birth because such infection causes the mother to release anti-inflammatory chemicals which, in turn, can trigger contractions. Smoking and the use of other teratogens can lead to preterm birth. A significant consequence of preterm birth includes respiratory distress syndrome, which is characterized by weak and irregular breathing.[8]
Small-for-date infants: Infants that have birth weights that are below expectation based on their gestational age are referred to as small-for-date. These infants may be full term or preterm, but still weigh less than 90 % of all babies of the same gestational age.
- This chapter was adapted from select chapters in Lumen Learning's Lifespan Development, authored by Martha Lally and Suzanne Valentine-French available under a Creative Commons Attribution-NonCommercial-ShareAlike license, and Waymaker Lifespan Development, authored by Julie Lazzara for Lumen Learning and available under a Creative Commons Attribution license. Some selections from Lumen Learning were adapted from previously shared content from Laura Overstreet's Lifespan Psychology. ↵
- Eisenberg, A., Murkoff, H. E., & Hathaway, S. E. (1996). What to expect when you’re expecting. New York: Workman Publishing. ↵
- American Pregnancy Association. (2015). Epidural anesthesia. http://americanpregnancy.org/labor-and-birth/epidural/ ↵
- Mayo Clinic. (2014). Labor and delivery, postpartum care. http://www.mayoclinic.org/healthy-lifestyle/labor-and-delivery/in-depth/inducing-labor/art-20047557 ↵
- Brazelton, T. B., & Nugent, J. K. (1995). Neonatal behavioral assessment scale. London: Mac Keith Press. ↵
- Centers for Disease Control and Prevention. (2015). Birthweight and gestation. http://www.cdc.gov/nchs/fastats/birthweight.htm ↵
- Centers for Disease Control and Prevention. (2015c). Preterm birth. http://www.cdc.gov/reproductivehealth/maternalinfanthealth/pretermbirth.htm ↵
- United States National Library of Medicine. (2015). Neonatal respiratory distress syndrome. https://medlineplus.gov/ency/article/001563.htm ↵

