Prenatal Development
Diana Lang; Martha Lally; Suzanne Valentine-French; Alisa Beyer; Julie Lazzara; and Naomi H. Dan Karami
Now we turn our attention to the three periods of prenatal development: the germinal period, the embryonic period, and the fetal period. While medical practitioners refer to trimesters, the three periods of prenatal development are stage based and are not equally distributed as 13-weeks each. Here is an overview of some of the changes that take place during each period.[1]
The Germinal Period (Weeks 0-3)

The germinal period begins from conception to the implementation of the zygote in the lining of the uterus, which lasts about 14 days. At ejaculation, a multitude of sperm are released into the vagina, and it only takes one sperm to fertilize the egg/ovum (Figure 1). When the egg ripens, it is released from the ovaries into the fallopian tube, which travels down to the uterus within 3-4 days, where the fertilization happens.
Immediately after the single sperm penetrates through the wall of the egg, the egg becomes hard and blocks other sperm from entering it. Only the sperm head, which carries genetic information from the male, can fuse with the nucleus of the egg. From there, a new cell forms, also known as a zygote, which contains genetic information from the male and female. During this time, the organism begins cell division and growth. After the fourth doubling, differentiation of the cells begins to occur as well. It is estimated that about 60 percent of natural conceptions fail to implant in the uterus. The rate is higher for in vitro conceptions.
Throughout this process, the organism begins cell division through mitosis. After five days of mitosis, there are 100 cells, which is now called a blastocyst. The blastocyst consists of both an inner and an outer group of cells. The inner group of cells (or embryonic disk) will become the embryo, while the outer group of cells, or trophoblast, becomes the support system, which nourishes the developing organism. Other cells develop to form the amniotic sac. The amniotic sac fills with a clear liquid (amniotic fluid) and expands to envelop the developing embryo, which floats within it. This stage ends when the blastocyst fully implants into the uterine wall.[2]
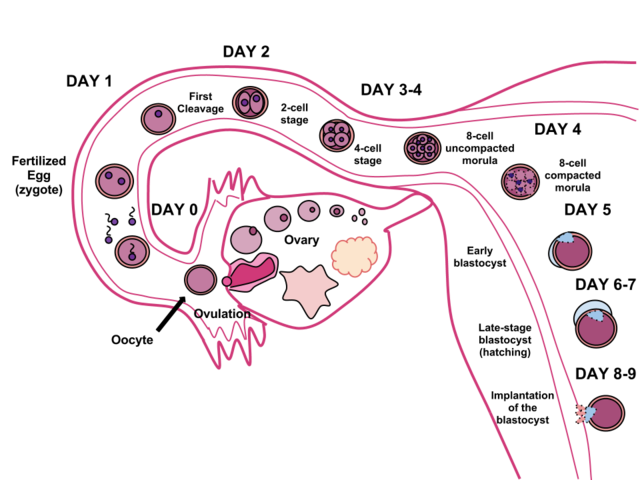
Less than one-half of all zygotes survive beyond the first two weeks.[3] One reason for this is outcome is that the egg and sperm do not join properly. As a result, their genetic material does not combine, there is too little or damaged genetic material, the zygote does not replicate, or the blastocyst does not implant into the uterine wall. The figure (2) below illustrates the journey of the ova from its release to its fertilization, cell duplication, and implantation into the uterine lining.
Watch this video on prenatal development:
It explains many of the developmental milestones and changes that happen during each month of development for the embryo and fetus.
The Embryonic Period (Weeks 3-8)

The embryonic period begins once the zygote is implanted in the uterine wall. It lasts from the third through the eighth week after conception. Upon implantation, this multi-cellular organism is called an embryo (figure 3). Now blood vessels grow, forming the placenta. The placenta is a structure connected to the uterus that provides nourishment and oxygen from the mother to the developing embryo via the umbilical cord.
During this period, cells continue to differentiate. Basic structures of the embryo start to develop into areas that will become the head, chest, and abdomen. During the embryonic stage, the heart begins to beat and organs form and begin to function. At 22 days after conception, the neural tube forms along the back of the embryo, developing into the spinal cord and brain.
Growth during prenatal development occurs in two major directions: from head to tail (cephalocaudal development) and from the midline outward (proximodistal development). This means that those structures nearest the head develop before those nearest the feet and those structures nearest the torso develop before those away from the center of the body (such as hands and fingers).
The head develops in the fourth week and the precursor to the heart begins to pulse. In the early stages of the embryonic period, gills and a tail are apparent. But by the end of this stage, they disappear and the organism takes on a more human appearance. The embryo is approximately 1 inch in length and weighs about 4 grams at the end of this period. The embryo can move and respond to touch at this time.
About 20 percent of organisms fail during the embryonic period, usually due to gross chromosomal abnormalities. As in the case of the germinal period, often the mother does not yet know that she is pregnant. It is during this stage that the major structures of the body are taking form making the embryonic period the time when the organism is most vulnerable to the greatest amount of damage if exposed to harmful substances. Potential mothers are not often aware of the risks they introduce to the developing child during this time.
The Fetal Period (Weeks 9-40)

When the organism is about nine weeks old, the embryo is called a fetus. At this stage, the fetus is about the size of a kidney bean and begins to take on the recognizable form of a human being as the “tail” begins to disappear (Figure 4).
From 9–12 weeks, the sex organs begin to differentiate. By the 12th week, the fetus has all its body parts including external genitalia. In the following weeks, the fetus will develop hair, nails, teeth and the excretory and digestive systems will continue to develop. At the end of the 12th week, the fetus is about 3 inches long and weighs about 28 grams.
At about 16 weeks, the fetus is approximately 4.5 inches long. Fingers and toes are fully developed, and fingerprints are visible. During the 4-6th months, the eyes become more sensitive to light and hearing develops. The respiratory system continues to develop. Reflexes such as sucking, swallowing, and hiccupping develop during the 5th month. Cycles of sleep and wakefulness are present at that time as well. Throughout the fetal stage, the brain continues to grow and develop, nearly doubling in size from weeks 16 to 28. The majority of the neurons in the brain have developed by 24 weeks although they are still rudimentary and the glial or nurse cells that support neurons continue to grow. At 24 weeks the fetus can feel pain.[4]
The first chance of survival outside the womb, known as the age of viability is reached at about 22 to 26 weeks.[5] By the time the fetus reaches the sixth month of development (24 weeks), it weighs up to 1.4 pounds. The hearing has developed, so the fetus can respond to sounds. The internal organs, such as the lungs, heart, stomach, and intestines, have formed enough that a fetus born prematurely at this point has a chance to survive outside of the mother’s womb.
Between the seventh and ninth months, the fetus is primarily preparing for birth. It is exercising its muscles, its lungs begin to expand and contract. It is developing fat layers under the skin. The fetus gains about 5 pounds and 7 inches during this last trimester of pregnancy, which includes a layer of fat gained during the eighth month. This layer of fat serves as insulation and helps the baby regulate body temperature after birth.
Around 36 weeks, the fetus is almost ready for birth. It weighs about 6 pounds and is about 18.5 inches long, and by week 37 all of the fetus’s organ systems are developed enough that it could survive outside the uterus without many of the risks associated with premature birth. The fetus continues to gain weight and grow in length until approximately 40 weeks. By then, the fetus has very little room to move around and birth becomes imminent (Figure 5).

Prenatal Brain Development
Prenatal brain development begins in the third gestational week with the differentiation of stem cells, which are capable of producing all the different cells that make up the brain.[6] The location of these stem cells in the embryo is referred to as the neural plate. By the end of the third week, two ridges appear along the neural plate first forming the neural groove and then the neural tube. The open region in the center of the neural tube forms the brain’s ventricles and spinal canal. By the end of the embryonic period, or week eight, the neural tube has further differentiated into the forebrain, midbrain, and hindbrain.
Brain development during the fetal period involves neuron production, migration, and differentiation. From the early fetal period until midgestation, most of the 85 billion neurons have been generated and many have already migrated to their brain positions. Neurogenesis, or the formation of neurons, is largely completed after five months of gestation. One exception is in the hippocampus, which continues to develop neurons throughout life. Neurons that form the neocortex, or the layer of cells that lie on the surface of the brain, migrate to their location in an orderly way. Neural migration is mostly completed by 29 weeks. Once in position neurons begin to produce dendrites and axons that begin to form the neural networks responsible for information processing. Regions of the brain that contain the cell bodies are referred to as the gray matter because they look gray in appearance. The axons that form the neural pathways make up the white matter because they are covered in myelin, a fatty substance that is white in appearance. Myelin aids in both the insulation and efficiency of neural transmission. Although cell differentiation is complete at birth, the growth of dendrites, axons, and synapses continue for years.
Teratogens
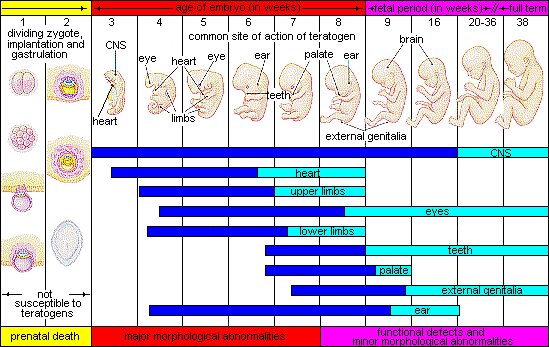
Quality prenatal care is essential. The developing embryo and fetus is most at risk for some of the most severe problems during the first three months of development. Unfortunately, most females are unaware that they are pregnant at this time. It is estimated that 10% of all birth defects are caused by a prenatal exposure or teratogen. Teratogens are factors that can contribute to birth defects which include some maternal diseases, drugs, alcohol, and stress. These exposures can also include environmental and occupational exposures. Today, we know many of the factors that can jeopardize the health of the developing child. Teratogen-caused birth defects are potentially preventable.
The study of factors that contribute to birth defects is called teratology. Teratogens are usually discovered after an increased prevalence of a particular birth defect. For example, in the early 1960s, a drug known as thalidomide was used to treat morning sickness. Exposure of the fetus during this early stage of development resulted in cases of phocomelia, a congenital malformation in which the hands and feet are attached to abbreviated arms and legs.
Factors influencing prenatal risks
There are several considerations in determining the type and amount of damage that might result from exposure to a particular teratogen (Figure 6).[7] These include:
- The timing of the exposure: Structures in the body are vulnerable to the most severe damage when they are forming. If a substance is introduced during a particular structure’s critical period (time of development), the damage to that structure may be more significant. For example, the ears and arms reach their critical periods at about six weeks after conception. If a woman exposes the embryo to certain substances during this period, the arms and ears may be malformed.
- The amount of exposure: Some substances are not harmful unless the amounts reach a certain level. The critical level depends in part on the size and metabolism of the mother.
Dose-response relation: The higher the exposure to the potential teratogen, the more likely it is that the fetus will suffer damage and the more severe the damage is likely to be with greater exposure. - Genetics: Genetic makeup also plays a role in the impact a particular teratogen might have on the child. This is suggested by fraternal twin studies who are exposed to the same prenatal environment, yet do not experience the same teratogenic effects. The genetic makeup of the mother can also have an effect; some mothers may be more resistant to teratogenic effects than others.
- Biological sex: Males are more likely to experience damage due to teratogens than are females. It is believed that the Y chromosome, which contains fewer genes than the X, may have an impact.
Paternal and Maternal Factors
Several factors can impact pregnancy and birth outcomes, such as paternal and maternal age, environmental teratogens, and the health conditions of both the male and female.
Paternal impact: The age of males at the time of conception is an important factor in health risks for children. According to Nippoldt,[8] offspring of males older than 40 years of age tend to have an increased risk of miscarriages, autism, birth defects, achondroplasia (bone growth disorder), and schizophrenia. These health risks are thought to be due to accumulated chromosomal aberrations and mutations during the maturation of sperm cells in older men.[9]
Maternal impact: Women who become pregnant at 35 years or older generally have healthy pregnancies. However, according to March of Dimes,[10]
women older than 35 years of age are at greater risk of:
- Fertility problems
- High blood pressure
- Diabetes
- Miscarriages
- Placenta previa
- Cesarean section
- Premature birth
- Stillbirth
- A baby with a genetic disorder or other birth defects
Exposure to environmental teratogens can affect the quality of eggs as women age and the quality of sperm from males. Women’s reproductive systems naturally age with time, which can have a significant negative impact on pregnancy, although a woman is born with all her eggs. For this reason, some women older than 35 years choose special prenatal screening such as blood screening to determine if there are any health risks for the baby.
Women who delay having children may live longer. Sun et al.[11] found that women who had their last child after the age of 33 years doubled their chances of living to age 95 or older when compared to women who had their last child before their 30th birthday. A woman’s natural ability to have a child at a later age indicates that her reproductive system is aging slowly, and consequently so is the rest of her body.
Prenatal Assessment
A number of assessments are suggested to women as part of their routine prenatal care to find conditions that may increase the risk of complications for the mother and fetus.[12] These can include blood and urine analyses and screening and diagnostic tests for birth defects.
Ultrasound is one of the main screening tests done in combination with blood tests. The ultrasound is a test in which sound waves are used to examine the fetus. There are two general types. Transvaginal ultrasounds are used early pregnancy, while transabdominal ultrasounds are more common and used after 10 weeks of pregnancy (typically, 16 to 20 weeks). Ultrasounds are used to check the fetus for defects or problems. It can also find out the age of the fetus, location of the placenta, fetal position, movement, breathing and heart rate, amount of amniotic fluid in the uterus, and number of fetuses. Most women have at least one ultrasound during pregnancy, but if problems are noted, additional ultrasounds may be recommended.
When diagnosis of a birth defect is necessary, ultrasounds help guide the more invasive diagnostic tests of amniocentesis and chorionic villus sampling. Amniocentesis is a procedure in which a needle is used to withdraw a small amount of amniotic fluid and cells from the sac surrounding the fetus and later tested. Chorionic villus sampling is a procedure in which a small sample of cells is taken from the placenta and tested. Both amniocentesis and chorionic villus sampling have a risk of miscarriage, and consequently they are not done routinely.
Complications of Pregnancy
Minor Complications
There are a number of common side effects of pregnancy. Not everyone experiences all of these, nor to the same degree. And although they are considered “minor” this is not to say that these problems are not potentially very uncomfortable. These side effects include nausea (particularly during the first 3-4 months of pregnancy as a result of higher levels of estrogen in the system), heartburn, gas, hemorrhoids, backache, leg cramps, insomnia, constipation, shortness of breath, or varicose veins (as a result of carrying a heavy load on the abdomen).
Major Complications
The following are some serious complications of pregnancy which can pose health risks to the woman and child and that often require hospitalization.
Ectopic pregnancy occurs when the zygote becomes attached to the fallopian tube before reaching the uterus. Sometimes and ectopic pregnancy occurs in the ovary, abdominal cavity, or the lower part of the uterus (cervix), which connects to the vagina.[13] Abdominal pain, vaginal bleeding, nausea, and fainting are typical symptoms of ectopic pregnancy.
Preeclampsia, also known as toxemia, is characterized by a sharp rise in blood pressure, a leakage of protein into the urine as a result of kidney problems, and swelling of the hands, feet, and face during the third trimester of pregnancy. Preeclampsia is the most common complication of pregnancy. Preeclampsia occurs most frequently in first pregnancies, and it is more common in women who are obese, have diabetes, or are carrying twins. When preeclampsia causes seizures, the condition is known as eclampsia, which is the second leading cause of maternal death in the United States. Preeclampsia is also a leading cause of fetal complications, which include low birth weight, premature birth, and stillbirth. Treatment is typically bed rest and sometimes medication. If this treatment is ineffective, labor may be induced.
Maternal mortality. Approximately 295,000 women died during and following pregnancy and childbirth in 2017. The vast majority of these deaths occurred in low-resource settings, and many could have been prevented.[14] Rates are highest in Subsaharan, Africa and South Asia, although there has been a substantial decrease in these rates. The campaign to make childbirth safe for everyone has led to the development of clinics accessible to those living in more isolated areas and training more midwives to assist in childbirth.
Spontaneous abortion is experienced in an estimated 20-40 percent of undiagnosed pregnancies and in another 10 percent of diagnosed pregnancies. Usually the body aborts due to chromosomal abnormalities, and this typically happens before the 12th week of pregnancy. Cramping and bleeding result and normal periods return after several months. Some women are more likely to have repeated miscarriages due to chromosomal, amniotic, or hormonal problems, but miscarriage can also be a result of defective sperm.[15]
- This chapter was adapted from select chapters in Development through the Lifespan, by Alisa Beyer & Julie Lazzara available under a Creative Commons Attribution-NonCommercial-ShareAlike license, Lumen Learning's Lifespan Development, authored by Martha Lally and Suzanne Valentine-French available under a Creative Commons Attribution-NonCommercial-ShareAlike license, and Waymaker Lifespan Development, authored by Sarah Carter and Sarah Hoiland for Lumen Learning and available under a Creative Commons Attribution license. ↵
- United States National Library of Medicine. (2015). Fetal development. https://www.nlm.nih.gov/medlineplus/ency/article/002398.htm ↵
- Hall, D. W. (2004). Meiotic drive and sex chromosome cycling. Evolution; International Journal of Organic Evolution, 58(5), 925–931. https://doi.org/10.1111/j.0014-3820.2004.tb00426.x ↵
- Royal College of Obstetricians and Gynecologists. (1997). Fetal Awareness: Report of a Working Party. London: RCOG Press. ↵
- Moore, K. L., & Persaud, T. V. (1998). Before we are born (5th ed.). Philadelphia, PA: Saunders. ↵
- Stiles, J., & Jernigan, T. L. (2010). The basics of brain development. Neuropsychology Review, 20(4), 327–348. https://doi.org/10.1007/s11065-010-9148-4 ↵
- Berger, K. S. (2005). The developing person through the life span (6th ed.). New York: Worth. ↵
- Nippoldt, T.B. (2015). How does paternal age affect a baby’s health? Mayo Clinic. http://www.mayoclinic.org/healthy-lifestyle/getting-pregnant/expert-answers/paternal-age/faq-20057873 ↵
- Bray, I., Gunnell, D., & Davey Smith, G. (2006). Advanced paternal age: how old is too old? Journal of Epidemiology and Community Health, 60(10), 851–853. https://doi.org/10.1136/jech.2005.045179 ↵
- March of Dimes. (2016). Pregnancy after age 35. http://www.marchofdimes.org/pregnancy-after-age-35.aspx ↵
- Sun, F., Sebastiani, P., Schupf, N., Bae, H., Andersen, S. L., McIntosh, A., Abel, H., Elo, I., & Perls, T. (2015). Extended maternal age at birth of last child and women’s longevity in the Long Life Family Study. Menopause: The Journal of the North American Menopause Society, 22(1), 26-31. ↵
- Eisenberg, A., Murkoff, H. E., & Hathaway, S. E. (1996). What to expect when you’re expecting. New York: Workman Publishing. ↵
- Mayo Clinic. (n.d.). Ectopic pregnancy. https://www.mayoclinic.org/diseases-conditions/ectopic-pregnancy/symptoms-causes/syc-20372088 ↵
- World Health Organization. (2019). Maternal mortality. https://www.who.int/news-room/fact-sheets/detail/maternal-mortality ↵
- Carrell, D. T., Wilcox, A. L., Lowry, L., Peterson, C. M., Jones, K. P., & Erikson, L. (2003). Elevated sperm chromosome aneuploidy and apoptosis in patients with unexplained recurrent pregnancy loss. Obstetrics and Gynecology, 101(6), 1229-1235. ↵

